Flaunt your Chest not Boobs
Call now & Get Discount: 8329060384
Best Gynecomastia Surgeon in Visakhapatnam (Vizag) Get Male Breast Reduction & Gland Removal from Best Surgeon!
Gynecomastia Male Breast Reduction Clinic in Visakhapatnam - Get the best treatment for Enlarged Male Breast, Puffy Nipples in India at very affordable cost. Complete guide on Gynecomastia, Causes, Symptoms, Cure and recovery. Find the best Male Breast Reduction Clinic in Visakhapatnam.
Call now & Get Discount: 9912493331
Free Consultation, Best Treatment, Lowest Cost, Easy Finance Available, 100% Result
Gynecomastia Surgery Cost in Visakhapatnam (Vizag) Know the Cost of Male Breast Reduction Surgery, Deals & Offers in Visakhapatnam (Vizag)
Gynecomastia Cost Depends on?
The cost of Gynecomastia Male Breast Reduction Surgery depends on Surgeon’s Qualification, Operative facilities, Technique of liposuction, Gland excision needed or not, Stay Required or not, Anaesthetist Experience, Type of Compression garment & Post care facilities given to patient.
Please fill the form for exact costing of Surgery in your condition.
Contact Us
We are located all over India, Our clinics are at Delhi, Gurgaon, Noida, Pune, Mumbai, Nagpur, Ahmedabad, Bangalore, Chennai, Hyderabad, Kolkata, Lucknow, Patna, Visakhapatnam and we are coming to more cities.
Please call:+91 8329060384
Find detailed information about Gynecomastia Causes, Symtoms, Diagnosis, Gynecomastia Grades, Candidates, Myths, Facts, Faq’s & Male Chest Reduction & Reshaping surgery in Visakhapatnam. If you are a Doctor from Visakhapatnam, You can request your profile on our website & If you are Gynecomastia patient you can find doctors, Ask your doubts about Male breast reduction or read the blogs. We have tried to list best Clinics, doctors & surgeons in & near Visakhapatnam. You can fill the form & submit your contact details to fix your free consultation with one of our affiliate doctors in Visakhapatnam. To know the approximate cost of Gynecomastia Treatment, click on - http://www.gynecomastiasurgery.co.in/gynecomastia-surgery-cost-financing/.
gynecomastia surgery emi, gynocamestia surgery, mens breast removal, puffy nipples male surgery cost, gynaecomastia surgery near me, gynecomastia surgery in vizag, men boobs operation, male breast reduction, men breast reduction, gynecomastia hospital near me, gynecomastia surgery cost in vizag, gynecomastia surgery doctor, gynecomastia doctor, best treatment for gynaecomastia, male gynecomastia surgery, gynecomastia surgery cost, man boob surgery, gynecomastia surgeon near me, gynecomastia surgery, chest fat surgery, gynecomastia treatment, man boobs removal, gynocomastia doctor, price of gynecomastia surgery, male breast surgery, mens nipple reduction cost, gynaecomastia surgery, gynecomastia treatment cost, breast reduction male, man boobs treatment, gynecomastia doctors near me, best gynecomastia surgeon near me, gynecomastia surgery cost in andhra pradesh, male breast reduction surgery cost, male chest reduction surgery, gynecomastia, puffy nipple surgery near me, gynecomastia solution
Male breasts can be a cause of embarrassment for men in their social circles and they can often be a subject of ridicule among their peers. However, they need not live with their male boobs or moobs all through their life. They can easily get rid of their breasts with a simple surgical procedure and if all goes well, this can be a permanent cure to it. The solution to this is gynecomastia surgery.
Gynecomastia surgery is a medical procedure to remove male breasts by expert doctors. Gynecomastia is a common problem among males and should not be a cause of worry as it is treatable. Also, with a simple surgical procedure followed by a couple of weeks of resting and healing, men can get rid of their breasts.
You can restore a naturally masculine form to your chest with the help of a trained, qualified cosmetic surgeon. With today's modern procedures, you can have a speedy operation, a quick recovery, and scars that are nearly undetectable.
It isn’t just a physical problem, rather its consequences are far-reaching. It can meddle with personality of a man, can cause low self-esteem and low confidence-level. There is a hesitation in wearing body-hugging clothes, in presenting one-self on a podium, and even in socializing. These things can lead to several psychological issues and inferiority complex within a person. For an overall well-being of a person, it is very important to lead a life which is respected and is free from such inferiority complexes.
Men who suffer from gynecomastia do not feel comfortable in their own skin and are often the laggards when it comes to dating, relationships or marriages. Physical intimacy with partner is hampered as these men feel embarrassed in taking off their clothes because of the fear of being either judged or rejected or both. A partner, in such case, should be considerate about gynecomastia and motivate the man to get it treated.
Therefore Gynecomastia surgery can be an easy solution to their relationship problems.
In Visakhapatanam, there are a number of people who are suffering from gynecomastia. In fact, world over, there is a large percentage of young males who have enlarged breasts. Men of Visakhapatnam are increasingly becoming conscious about their appearances and overall personality. There has been an upshot in those who are visiting cosmetic surgery centers in their city to get rid of male breasts. There are a number of gynecomastia surgery options available in Visakhapatnam. Gynecomastia surgery in Visakhapatnam is a safe and secure procedure and is carried out by expert doctors and under proper medical supervision. There shouldn’t be any hesitation and fear among men regarding gynecomastia surgery. Visakhapatnam is a city that is rapidly developing and has advanced medical facilities. Surgery of gynecomastia is done in Visakhapatnam and is being opted by a number of men and teenage boys who have enlarged breasts.
Gynecomastia: What is it?
Gynecomastia is a condition in which a hormonal imbalance between estrogen and testosterone causes an increase in the amount of breast gland tissue in boys and men. Gynecomastia can affect one or both breasts, and it has varied effects on each. Breast enlargement is another name for it. A condition known as pseudogynecomastia occurs when a man's breasts grow some fat but not glandular tissue.
Natural hormonal changes can produce gynecomastia in infants, boys going through puberty, and older men, though there are other causes as well.
It is important to remember that gynecomastia is not a serious medical condition, but it can be distressing for individuals because it can be unpleasant at times.
What causes Gynecomastia in men?
The primary reason behind why men develop breasts like women, is hormonal imbalance. Clearly, such an imbalance can cause a swollen male breast tissue.
Male breast tissue bulges when male hormones (testosterone) are reduced or feminine hormones are raised (estrogen). Some of the causes include puberty, ageing, medicine, and health concerns that affect hormones.
Experts have pointed out that most dairy and meat animals are treated with for faster and better meat and milk production, and that consuming such products causes hormonal imbalance.
Even gym-goers' nutritional supplements are tainted with steroids, which might interfere with the generation of androgens. As a result of the increased relative activity of estrogens, males who take steroid-laced supplements get larger breasts.
Facts about gynecomastia
According to studies, the prevalence of this breast enlargement issue among men has increased in the country, and it is more widespread among guys aged 19 to 25. Even in the middle-aged population, however, there are some incidences of gynecomastia.
The problem is significantly more prevalent in adolescent boys. According to recent studies, about 80% of adolescent boys have gynecomastia, but because it is mostly a developmental issue, it usually goes away on its own. However, due to a variety of causes, it remains in roughly 10% to 20% of cases.
Gynecomastia treatment
While reducing weight can help some men lessen the appearance of male breasts, there is often excess glandular tissue present, causing even the slim patients to notice enlarged breasts. Male breast reduction is currently the only consistently effective gynecomastia treatment with long-term, if not permanent, outcomes. Patients frequently describe feeling comfortable being naked for the first time in years after this operation, as well as an increased sense of self-confidence.
Because of the fact that it is so effective and provides so many benefits, male breast reduction is one of the best therapies for gynecomastia. In Visakhapatnam, you may contact gynecomastia experts and book an initial consultation to see if this surgery is suitable for you. The experts assess the severity of your illness, as well as your medical history, current health, and goals, in order to devise the safest and most successful treatment plan for you.
Gynecomastia surgery: all you need to know
If medicinal treatment for chronic gynecomastia fails, glandular breast tissue must usually be removed surgically. Surgery is the "most effective known treatment for gynecomastia," according to the American Board of Cosmetic Surgery. Subcutaneous mastectomy, liposuction-assisted mastectomy, laser-assisted liposuction, and laser-lipolysis without liposuction are all surgical options for treating hypertrophy. Hematoma, surgical wound infection, breast asymmetry, changes in breast feeling, necrosis of the areola or nipple, seroma, visible or painful scars, and shape deformities are all possible complications of mastectomy.
Before the surgery actually takes place, the patient is advised to do a full research on the condition. One must also consult only an expert in this field.
There is a session of initial consultancy, wherein the experts will ask you detailed questions about your problem. They will then give you a chance to tell them what your expectations from the treatment option are. They will counsel you about the surgery, the process, the expense involved, and the risk factors involved (if any). The final decision about whether or not to proceed with the surgery lies in your hands.
The entire process is then conducted in a very safe and reliable environment under proper medical supervision by the experts. The treatment involves removal of the excess of fat (breast tissue).
Male breast reduction involves the removal of fat and glandular tissue from the breasts, as well as excess skin in extreme cases, to produce a flatter, firmer, and better-shaped chest. After liposuction, asymmetry, dimpling, wrinkling, unevenness, and surface irregularities might arise. It can be avoided using VASER (Vibration Amplification of Sound Energy at Resonance). In order to achieve comprehensive body contouring in men, male breast reduction is usually combined with VASER lipo of the abdomen, flanks, and back.
The outcomes of a gynecomastia breast reduction are considered permanent. The fat cells in the chest cannot grow back once they have been eliminated. However, depending on your genetics, the residual fat cells in your chest may enlarge if you gain a significant amount of weight in the future. You will not develop any more glandular tissue in your chest if the underlying cause of your gynecomastia, such as hormone abnormalities, was correctly detected and treated.
When conducted by experienced surgeons, gynecomastia surgery is a reliable therapy. Even though it is regarded as a permanent solution, recurrence is possible; but since the main causes, fat and glandular tissues, are removed, the chances of recurrence are quite low.
The surgery is a daycare process and there isn’t any need for the patient to remain in hospital after the procedure. The patient can get discharged the same day, once he feels alright post the surgery.
Therefore, it is carried out on an outpatient basis under local anesthesia and sedation or general anesthesia.
In the weeks following the surgery, there can be a need to be careful and watchful. The patient will be given a compression vest in the initial week after the surgery which helps to support the skin and will also work to prevent any accumulation of fluid.
There may be some swelling and bruising and other surgical aftereffects which may subside after medications.
The patients need to be watchful of their diet in the coming weeks and be regular with their medicines. Any kind of physical activity and exercising must be avoided in the initial weeks. The patient should take as much rest as he can. In the later weeks, if the doctor permits, the patient can resume daily activities like going to work and coming back home. However, even during this time strenuous activity must be avoided at all costs. You need to give time to your surgery to heal. Always remember, before starting physical activities it is important to have a consultation with your doctor. Also, it is advised to remain in touch with the doctor all through the recovery process.
Gynecomastia patients are strictly advised to refrain from smoking marijuana and drinking alcohol. They also must avoid taking anabolic steroids unless prescribed by doctor, as they may meddle with the hormonal balance of the body.
Positive changes after gynecomastia surgery:
Be ready to welcome a wonderful life again in a new avatar after gynecomastia treatment. The new you would be a confident and an attractive person. You will begin to feel comfortable in your own skin once you get rid of male breasts once and for all. The treatment makes the personality more attractive and likeable.
Gynecomastia does a lot more of psychological and social damage rather than harming your health. It is to be noted that gynecomastia isn’t a serious health hazard, but its timely recognition and treatment can help patients avoid a whole series of social contempt and derision, which may further aggravate into serious mental conditions like anxiety, low self-esteem. In the worst cases this may worsen into depression. Men shouldn’t be shy to talk about their problem of gynecomastia. In fact, they can consult the correct doctor and tell everything openly to them.
There would be some instances when you would feel like wearing fashionable clothes but have to make-do with baggy clothes because of the enlargement of your breasts. Now, baggy clothes do not fit everywhere, especially in corporate offices which require employees to be highly presentable all the times. Thus wardrobe is always an issue with those suffering from gynecomastia. After the surgery , your issue with shopping and your wardrobe will significantly disappear. You can now shop for whatever design and size of clothes you want. When you wear clothes that fit your new, masculine figure following breast reduction for gynecomastia correction, you'll feel more at ease, look more confident, and attract a lot more of the proper sort of attention.
Gynecomastia surgery in Visakhapatnam:
In Visakhapatnam, there are a number of options which are coming up for gynecomastia treatment. Gynecomastia surgery in Visakhapatnam is being sought increasingly by young men, teenage boys and even older men who have developed gynecomastia. The treatment options available here are safe, viable, affordable and have lasting outcome.
Gynecomastia surgeons in Visakhapatnam are experienced doctors who perform the entire process with great precision.
Therefore, do not hesitate, go ahead for gynecomastia surgery and get rid of it to finally embrace your masculinity.
Visakhapatnam district is a district in the Indian state of Andhra Pradesh. It is one of the nine coastal districts in the state, with the administrative headquarters located at Visakhapatnam. The district has four revenue divisions, namely Anakapalli, Paderu, Narsipatnam and Visakhapatnam, each headed by a sub collector. These revenue divisions are divided into 43 mandals in the district. These district consists of 3265 villages and 15 towns including, 1 municipal corporation, 2 municipalities and 12 census towns. Visakhapatnam city is the only municipal corporation and the 3 municipalities in the district are Anakapalle, Bheemunipatnam and Narsipatnam. The 12 census towns are Bowluvada, Chodavaram, Chintapalle, Gudivada, Kantabamsuguda, Mulakuddu, Nakkapalle, Narsipatnam, Peda Boddepalle, Payakaraopeta, Upper Sileru Project Site Camp, Yelamanchili. The total of core road network of the district is 945.443 km (587.471 mi). It includes, 298.783 km (185.655 mi) of existing and a proposed length of 646.660 km (401.816 mi).
The information on this site is intended for general purposes only and is not intended to nor implied to be a substitute for professional medical advice relative to specific medical conditions or questions. The information on this website is not a guide to treatment, and it should not replace seeking medical advice from your physician. We do not warrant the accuracy, completeness, correctness, timeliness or usefulness of any information contained herein. In no event Domain.com be liable to anyone for any decision made or action taken in reliance upon the information provided through this website. The photos on this website are of models & are not intended to represent the results that every patient can expect. Surgical results vary greatly from patient to patient and are not guaranteed.
Gynecomastia can be termed as: “The enlargement of excess breast tissue in men”. It can be significant amount of embarrassment, especially when changing in public or swimming.
This is very common situation which occurs between 32% to 40% of men population and 65% during puberty. Sometimes Gynecomastia will go away on its own, as most cases are associated with puberty, whereas in a small minority of men it becomes permanent.
Who Is A Good Candidate For Male Breast Reduction (Gynecomastia) Surgery?
Men with any of the following may be candidates for male breast reduction surgery in Visakhapatnam:
- Have firm, elastic skin
- Are over 18 years of age
- Are not obese
- Are not taking steroids or recreational drugs
- Have excess fat tissue that does not respond to diet, exercise, or medical treatments
- Are self-conscious about their appearance due to gynecomastia
- Do not smoke or use alcohol excessively
How is a male breast reduction performed in Visakhapatnam?
Various techniques can be adopted by the different surgeons for obtaining the perfect contour depends on the amount of surplus gland, fat, and skin present.
“Liposuction of Male breast” is only one of the main surgical treatment is available for the Gynecomastia problem. The majority of men can be treated with liposuction alone.
A small incision around the areola is needed to remove the excess glandular tissues. Sometimes a combination of gland excision and liposuction is needed to obtain optimal results. Where the larger amount of excess gland, fat and skin is there in these cases, larger incisions may be needed to obtain a flat chest contour. Chest hair and the areola help to hide these incision scars.
Surgeon will recommend you what technique will be the best for your body contour.
Recovery after Male Breast Reduction Surgery:
Generally after surgery there will be some swelling and brushing for couple of weeks which is very normal. Doctor will refer you to wear the compression garment which will help you a lot to reduce the swelling and the brushing as early as possible. You need to wear those garments at least 1-2 months depending upon the amount of tissues removed.
Most men feel well enough to go back to work within 7 to 10 days. Doctor will see you regularly after your male breast reduction surgery to ensure that you’re healing well and progressing well.
Notable Facts about Gynecomastia
Frequently a brief condition: In by far most of instances of growth of the male breast (Gynecomastia) the condition is transitory and it as a rule happens amid the adolescence (ages: 13 to 18). Assuming, in any case, the condition perseveres after the high school years then the possibility of this condition being changeless turns out to be to a greater extent a worry. For evident delicate reasons this condition is once in a while discussed. Gynecomastia is entirely normal and influences 40 to 60 per cent of men. Most guys that look for treatment are between the ages of 18 to 50. They for the most part show that they were ignorant of some other relatives having the condition and they relate a background marked by dodging conditions that require an uncovered chest. I.e. swimming with a "T" shirt on or keeping away from the young men's shower after a football game. They are generally solid and are on no drug that may have caused this condition. On examination these males fall into two principle classes:
One who is a 24 year old active male who notices enlargement of his breasts during the stage of puberty and the condition is worsened into his young adult years and who usually makes a statement that there is a firm mass of fat that he feels beneath his nipples.
Second who belongs to the age of 35 to 50 years and currently notices enlargement of his breasts since the age of 40 years. He acknowledges that over the past few years he has put up some weight and complains of his chest expansion and to conceal this situation he prefers to wear large sized shirts so that he doesn’t have to embarrass himself in front of others.
- Breast tumours which generally involve one breast, the side effects those medications can have leading to enlargement of male breasts; the medications can be of various types such as etc. these are some of the most common causes of Male Breast Enlargement. Apart from those, drugs such as marijuana, heroin and alcohol or natural aging, obesity, changes in hormones during puberty can also lead to gynecomastia.
- The candidates that are most suited for gynecomastia correction are recently not practicing any of the above mentioned medication and hence a breast tumour can be ruled out of the scenario. Once the excess breast tissue is taken out these males have a firm and elastic skin that reshapes to the new contour of the body.
Male Breast Reduction- Procedure:
Usually the incisions are hidden within the dark part of the nipple. So as to ensure confidentiality of the procedure most of it can be done in an office setting itself.
The soporific of decision is a mellow I.V. sedation in addition to a neighbourhood soporific of the chest.
The method takes around 1 ½ hours to perform and there are weight lifting confinements for around 2 weeks a short time later.
Gynecomastia is defined as an increase in the size of the mammary gland in men. It corresponds to unilateral or bilateral hyperplasia. Usually it is idiopathic, that is to say that there is no cause for its occurrence; however, in some cases it may be related to abnormal hormone production, or to taking certain medications. A workup is necessary in order to rule out a possible cause. The purpose of this assessment will be to measure the different known hormones, to look for a testicular or pituitary tumor. A mammogram or ultrasound may be requested in order to analyze the density of the gland, or eliminate breast cancer in older men, especially in the unilateral form. If a cause is found, it should be the subject of specific treatment. Indeed, when an etiology is found, the treatment of this one can allow a more or less complete regression of the gynecomastia.
The increase in breast volume in men, especially during adolescence, is often badly experienced and can cause many psychological problems. This physical attack in the adolescent, at the very moment when he is constructing his image as a man, can lead to a withdrawal into himself, or even a real complex. In addition, this gynecomastia can be painful.
From an anatomical and pathophysiological point of view, the mammary gland exists in normal humans, but it is of the infantile type, reduced to a simple breast bud. In a few cases, this mammary gland can develop if the hormonal environment is right.
When no cause has been found and if the patient is embarrassed, surgical intervention may be proposed, provided the patient is in good physical and mental condition. This type of intervention is called a "gynecomastia cure".
What does gynecomastia look like?
It is a development of the mammary gland centered on the areola, most often bilateral and symmetrical, of firm consistency and sensitive to palpation. Gynecomastia should be distinguished from adipomastia which is much more frequent and corresponds to a local accumulation of fat. These adipomasties are not centered in relation to the areola, their consistency is soft, insensitive, bilateral, symmetrical, but the two can be associated (adipogynecomastia).
In adolescents, transient gynecomastia may appear, linked to a hormonal imbalance in favor of estrogen, which disappears within a few months.
Breast cancers have a different presentation; it is a rare form, usually affecting men after 40 years. These are unilateral, hard, insensitive lesions associated with deformities or retractions of the nipple or even a bloody discharge.
What are the objectives of this intervention?
The goal of corrective surgery is to restore normal anatomy as much as possible with the following principles:
- reduce breast volume by direct surgical excision (subcutaneous mastectomy) for glandular forms, or by liposuction for fatty forms. In the case of mixed forms, the surgeon must then combine the two techniques,
reduce excess skin: generally, the decrease in glandular volume will allow skin retraction. This skin retraction is favored by the liposuction but it is all the more clear that it is a young man and that the skin is of good quality (firm, elastic skin, without stretch marks). Certain post-operative actions such as massages can help skin retraction.
In some cases, when the excess skin is too large, the surgeon may have to reduce it, but at the cost of scarring on the skin. This skin reduction plasty can be performed from the first intervention or secondarily.
gynecomastia surgery
gynecomastia surgery cost
gynecomastia treatment
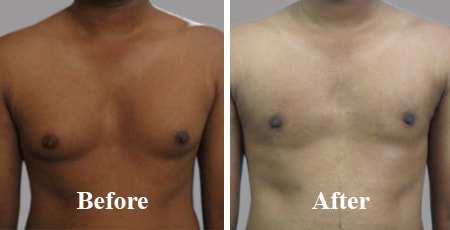
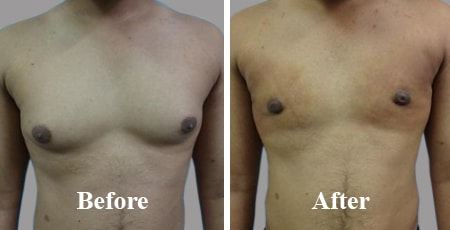
Tags: Gynecomastia Symptoms in Visakhapatnam, Gynecomastia Causes in Visakhapatnam, Gynecomastia Before And After Surgery in Visakhapatnam, Gynecomastia Surgery Near Me in Visakhapatnam, Treating Gynecomastia Without Surgery, Gynecomastia Removal in Visakhapatnam, How Much Gynecomastia Surgery in Visakhapatnam, Gynecomastia Grades in Visakhapatnam, Gynecomastia Cure in Visakhapatnam, Gynecomastia Doctors in Visakhapatnam, Gynecomastia Post Surgery in Visakhapatnam, Gynecomastia Liposuction in Visakhapatnam, Gynecomastia Reduction in Visakhapatnam, Gynecomastia In Children in Visakhapatnam, Gynecomastia Free Consultation
What does the intervention consist of?
In the typical procedure, an incision is made at the lower edge of the areola. From this incision, the surgeon can remove the mammary gland (subcutaneous mastectomy) and excess fat. Often in addition to this gesture, the surgeon can practice a liposuction at the periphery of the glandular excess in order to harmonize the whole.
In the case of predominantly fatty gynecomastia, the excision can sometimes be done by liposuction alone. The scars are then very short and can be located at a distance from the gynecomastia, such as in the sub-mammary or axillary regions.
When the gynecomastia and the excess skin are very important, the surgeon may have to make the scars longer and therefore more visible. These scars can then be peri-nipple (around the areola), horizontal and extend on either side of the areola. In extreme cases, the surgeon may have to transplant the areola and the nipple. Other types of scars are possible (vertical, racquet tail…), they depend on each particular case.
During the operation, a drain can be put in place depending on the technique used and the surgeon's habits. This drain is used to evacuate blood and lymphatic residues that could accumulate at the operating site.
At the end of the operation, a "modeling" dressing is made, often with an elastic bandage.
What type of anesthesia will I need?
This is a classic general anesthesia, during which you sleep completely.
How long will the intervention last?
the procedure usually lasts between 1 and 3 hours
How long will I be hospitalized?
Hospitalization for 24 hours is usually necessary. The length of hospital stay, however, depends on the surgical technique used. Indeed, a simple liposuction will require a shorter hospital stay than a subcutaneous mastectomy.
In some cases, the operation can be performed on an "outpatient basis", that is to say with an exit the same day after a few hours of monitoring.
What should I do before the procedure?
he assessment to find a cause for gynecomastia has been mentioned previously.
In obese or overweight men, a diet associated with physical exercises is initiated because weight loss can regress or even eliminate gynecomastia (adipomastia). Depending on the anatomical context, the preferences and habits of the surgeon, and the wishes expressed by the patient, an operating strategy will have been decided. The operative technique used and the location of the scars will thus be predetermined.
A usual preoperative assessment is carried out in accordance with the prescriptions. The anesthetist will be seen in consultation, at the latest 48 hours before the operation. Your surgeon and the anesthetist will need to be kept informed of all the medications you are taking. Indeed, some of them can interfere with the anesthesia or promote bleeding.
Except in special cases, no medication containing aspirin or anti-inflammatory drugs should be taken in the ten days preceding the operation.
Stopping smoking is recommended at least one month before and one month after the operation (tobacco can be the cause of delayed healing).
How does it work after the intervention?
The postoperative effects can sometimes be painful during the first few days. Analgesic treatment, adapted to the intensity of the pain, will be prescribed for a few days. In the event of isolated liposuction, the patient may locally experience pain in the type of "severe stiffness". Edema (swelling), bruising (bruising) and difficulty raising the arms are common at first.
The first dressing is removed after a few days. It is then replaced by a lighter dressing. Often, the initial dressing is compressive, then quickly a lighter dressing is combined with a compression vest to be worn day and night for a period of time. This retention helps skin retraction and promotes uniform healing.
The total length of time off work varies from five to twenty-one days. It is advisable to wait one to two months before resuming a sporting activity
What will be the result of the intervention?
The improvement is often clear and immediate. However, a period of two to three months is necessary to assess the final result. This is the time needed for the postoperative edema to disappear and the excess skin to retract. Beyond this period, the tissues will gradually gain flexibility.
The reduction in breast volume brings physical comfort, especially when getting dressed. Finally, the result is often very beneficial on the psychological level because gynecomastia is often considered as a shadow to virility.
As regards the stability of the result, several cases are possible. For pure glandular forms, glandular excision generally prevents recurrence. However, significant weight gain may be accompanied by a further increase in breast volume (adipomastia) and this is all the more common for forms with a predominant fatty component.
Can there be imperfections?
Some imperfections can occasionally be encountered:
- a residual asymmetry of volume: it can be due to a less important resection on one side than on the other, in particular when there was already an asymmetry of volume before the operation. In some cases, the asymmetry can be linked to a more important postoperative edema on one side: in this case, wearing a sheath and the action of massages will correct the defect. When the asymmetry persists one year after the operation and if it is troublesome, surgical correction may then be proposed.
- asymmetry in the height of the areolas and nipples: the asymmetry is often present before the operation; however, you paid little attention or even didn't notice it. After the operation, even if the surgeon has tried to correct it, the asymmetry can persist and sometimes be "unmasked", ie made more visible.
In other cases, the asymmetry may be related to the scarring of the tissues under the skin. Daily massages combined with good hydration will help correct the problem. - cupulation of the areola: it can be linked to a glandular excision too centered behind the areola without peripheral harmonization. If it is bothersome, surgical retouching may be proposed.
- excess skin: after surgical correction of gynecomastia, excess skin is not uncommon and can take several months to retract. Skin retraction is related to the quality of the skin. Touch-up may be desirable.
- hollow areas or small nodules under the skin: these are linked to liposuction which in some cases can increase the appearance of "cellulite". This phenomenon is normal: daily massages combined with good hydration will allow these fibrous nodules to be broken up and prevent deep adhesions (appearance of "cellulite").
- As for the issue of the evolution of scars, it was mentioned previously.
The tenderness of the nipples is usually not affected, or transiently for a few months. Insensitivity is exceptional. On the other hand, when the surgeon has to graft the areolo-nipple plaque, the latter may become permanently insensitive and may present skin color disorders (dyschromia).
What are the possible risks and complications?
Although a gynecomastia cure is carried out for essentially aesthetic reasons, it is nonetheless a real surgical intervention, which involves the risks associated with any medical act, however minimal.
The operative consequences are generally simple after a cure for gynecomastia. However, complications can arise, some of a general nature, inherent in any surgical procedure, others more specific loco-regional of the treatment of gynecomastia.
It is necessary to distinguish the complications related to anesthesia from those related to the surgical procedure.
Regarding anesthesia, during the compulsory pre-operative consultation, the anesthetist himself will inform the patient of the anesthetic risks. You should know that anesthesia induces reactions in the body that are sometimes unpredictable and more or less easy to control: the fact of having recourse to a perfectly competent anesthesiologist, working in a truly surgical context, that the risks incurred have become statistically extremely weak.
It should be kept in mind that techniques, anesthetics and monitoring methods have made immense progress over the last thirty years, offering optimal safety, especially when the intervention is performed outside of the emergency. in a healthy person.
With regard to the surgical procedure, by choosing a qualified and competent Plastic Surgeon, trained in this type of intervention, you limit these risks as much as possible, without however completely eliminating them.
In practice, the vast majority of gynecomastia cures performed correctly go without any problems. The postoperative follow-up is straightforward and patients are fully satisfied with their results. However, sometimes complications can still arise:
- Postoperative bleeding and hematoma: bleeding may occur in the hours following the operation. If it is important, it will result in swelling and painful tension (hematoma) and will require evacuation.
- Phlebitis and pulmonary embolism: resuming walking very early can minimize this risk.
- Serous effusion: An accumulation of lymphatic fluid in the area of mastectomy is sometimes observed. We also talk about lymphocele or seroma. It may require one or more punctures in order to evacuate it.
- Postoperative infection: it can appear in the days following the operation and results in a fever, sometimes above 39 ° C. The operated area is then swollen and red, painful. Antibiotic treatment may be sufficient, but often surgical drainage is necessary.
- Skin necrosis: the skin needs a good vascular supply (oxygen supply) to live. If the vascularization is insufficient or of poor quality (significant traction, hematoma, infection, smoking, etc.), skin necrosis may occur. It will be treated with appropriate care and dressings. Healing will be obtained but with a certain delay.
- Pneumothorax: very rare, it will benefit from specific treatment.
- Abnormal scars: the surgeon does his best to make good sutures; however, scarring is a random occurrence and sometimes the scars are not as subtle as desired. In the same person, depending on the region of the body, healing may be different. Thus, the evolution of scars can be unfavorable with the occurrence of hypertrophic scars, even keloids, of unpredictable appearance and development, which can compromise the aesthetic appearance of the result and require specific local treatments which are often long.
- Skin sensitivity disorders: an alteration in skin sensitivity is common during the first few months and then subsides before returning to normal. Rarely, can appear bad sensory information with exaggeration of the sensitivity; these particular cases require specific treatment. As we have seen previously, when the surgeon has to graft the areolo-nipple plate, it can remain permanently insensitive.
All in all, we should not overestimate the risks, but simply be aware that a surgical intervention, even seemingly simple, always involves a small share of risks.
Recourse to a qualified Plastic Surgeon assures you that this one has the training and the competence required to know how to avoid these complications or to treat them effectively if necessary.
Will this intervention be covered by Social Security?
Depending on the case, this intervention may be partially covered by the Health Insurance.