Flaunt your Chest not Boobs
Call now & Get Discount: 8329060384
Best Gynecomastia Surgeon in Lucknow Get Male Breast Reduction & Gland Removal from Best Surgeon!
Gynecomastia Male Breast Reduction Clinic in Lucknow - Get the best treatment for Enlarged Male Breast, Puffy Nipples in India at very affordable cost. Complete guide on Gynecomastia, Causes, Symptoms, Cure and recovery. Find the best Male Breast Reduction Clinic in Lucknow.
Call now & Get Discount: 8329060384
Free Consultation, Best Treatment, Lowest Cost, Easy Finance Available, 100% Result
Gynecomastia Surgery Cost in Lucknow Know the Cost of Male Breast Reduction Surgery, Deals & Offers in Lucknow
Gynecomastia Cost Depends on?
The cost of Gynecomastia Male Breast Reduction Surgery depends on Surgeon’s Qualification, Operative facilities, Technique of liposuction, Gland excision needed or not, Stay Required or not, Anaesthetist Experience, Type of Compression garment & Post care facilities given to patient.
Please fill the form for exact costing of Surgery in your condition.
Contact Us
We are located all over India, Our clinics are at Delhi, Gurgaon, Noida, Pune, Mumbai, Nagpur, Ahmedabad, Bangalore, Chennai, Hyderabad, Kolkata, Lucknow, Patna, Visakhapatnam and we are coming to more cities.
If you have questions or need additional information, please call:+91 8329060384 or use our Contact Form!
Find detailed information about Gynecomastia Causes, Symtoms, Diagnosis, Gynecomastia Grades, Candidates, Myths, Facts, Faq’s & Male Chest Reduction & Reshaping surgery in Lucknow. If you are a Doctor from Lucknow, You can request your profile on our website & If you are Gynecomastia patient you can find doctors, Ask your doubts about Male breast reduction or read the blogs. We have tried to list best Clinics, doctors & surgeons in & near Lucknow. You can fill the form & submit your contact details to fix your free consultation with one of our affiliate doctors in Lucknow. To know the approximate cost of Gynecomastia Treatment, click on - http://www.gynecomastiasurgery.co.in/gynecomastia-surgery-cost-financing/.
chest fat surgery, male breast reduction, gynecomastia surgery in kanpur, male breast reduction surgery, gynecomastia doctor, gynecomastia doctors near me, gynecomastia surgery cost in lucknow, gynecomastia surgery in varanasi, low cost gynecomastia surgery, surgery of gynecomastia, gynecomastia surgery near me, gynecomastia removal, gynecomastia surgery, gynecomastia gland removal, gynecomastia treatment, gynecomastia best doctor, gynecomastia cost, gynecomastia surgery hospital, gynecomastia surgery in gorakhpur, gynecomastia surgery prices, chest fat surgery cost, breast reduction, man chest fat, gynecomastia surgery cost, gynecomastia doctor in lucknow, gynecomastia treatment hindi, men boobs reduction, gynecomastia surgery cost in kanpur, men boobs problem, gynaecomastia treatment, cost of gynecomastia surgery, moobs reduction, gynecomastia hospital near me, gynecomastia surgery price, gynecomastia doctor near me, gynecomastia best treatment, men boobs surgery, chest fat loss, gynecomastia treatments, doctor for gynecomastia near me, gynecomastia treatment in hindi, gynecomastia surgery in lucknow, gynecomastia specialist, gynecomastia surgeon near me, गाइनेकोमैस्टिया सर्जरी
Lucknow district is a district located in the Uttar Pradesh state in northern India. The city of Lucknow is the district headquarters and the district is part of Lucknow Division and also is the capital of Uttar Pradesh. Blocks in Lucknow District - The following are the blocks in the district of Lucknow: Bakshi Ka Talab, Chinhat, Gosainganj, Kakori, Mal, Malihabad, Mohanlalganj, Sarojini Nagar. The district has five tehsils, Sadar, Mohanlalganj, Bakshi ka Talab, Malihabad and Sarojni Nagar. Two major Indian National Highways have their intersection at Lucknow's Hazratganj intersection: NH-24 to Delhi, NH-30 to Allahabad via Raebareli, NH-27 to Porbandar via Jhansi and Silchar via Gorakhpur. Lucknow city's bus service is operated by Uttar Pradesh State Road Transport Corporation (UPSRTC). The major Dr. Bhimrao Ambedkar Inter-state Bus Terminal (ISBT) in Alambagh provides the main inter and intrastate bus lines in Lucknow. Main cities served by the UPSRTC intrastate bus service are Allahabad, Varanasi, Jaipur, Agra, Delhi, Gorakhpur. The cities outside Uttar Pradesh that are covered by inter-state bus services are Jaipur, New Delhi, Gwalior, Bharatpur, Singrauli, Faridabad, Gurgaon, Dausa, Ajmer, Dehradun, and Haridwar. Lucknow is served by several railway stations in different parts of the city. The main long-distance railway station is Lucknow Railway Station located at Charbagh. The city is an important junction with links to all major cities of the state and country such as New Delhi, Mumbai, Hyderabad, Kolkata, Chandigarh, Amritsar, Jammu, Chennai, Bangalore, Ahmedabad, Pune, Indore, Bhopal, Jhansi, Jabalpur, Jaipur and Siwan.
The information on this site is intended for general purposes only and is not intended to nor implied to be a substitute for professional medical advice relative to specific medical conditions or questions. The information on this website is not a guide to treatment, and it should not replace seeking medical advice from your physician. We do not warrant the accuracy, completeness, correctness, timeliness or usefulness of any information contained herein. In no event Domain.com be liable to anyone for any decision made or action taken in reliance upon the information provided through this website. The photos on this website are of models & are not intended to represent the results that every patient can expect. Surgical results vary greatly from patient to patient and are not guaranteed.
Gynecomastia, Enlarged Male Breasts.
Gynecomastia is a restorative term that starts from the Greek words for "ladies like breasts." This condition is significantly more typical than numerous figure it out. Gynecomastia influences an expected 40 to 60 per cent of the male populace. It might influence just a single breast or both. Albeit certain medications, for example, anabolic steroids, medicines containing ESTROGEN, liquor, marijuana, and so forth., and therapeutic conditions including malignancy, weakened liver capacity, to give some examples, may cause or add to developed male breasts, it is broadly acknowledged that a huge level of cases get from obscure sources.
Men of all ages who are sound and sincerely stable are viewed as great contender for male breast diminishment medical procedure. The best applicants are the individuals who have firm, flexible skin that will reshape to the body's new shapes. In a few cases, medical procedure might be disheartened for overweight men who have not first attempted an activity and eating routine regimen.
Amplified male breasts can be diminished by liposuction and additionally by removing abundance glandular tissue. The technique for male breast lessening takes a normal of two hours, more often than not on an outpatient premise, utilizing general or neighbourhood anaesthesia. In the event that unreasonable glandular tissue, fat and skin is available, it will be evacuated.
Medical procedure might be performed alone or in conjunction with lipoplasty, where the suction gadget will regularly be embedded through the current entry points. For the evacuation of abundance greasy tissue alone, liposuction might be all that is required; in such cases, scars will be little and scarcely obvious. Results are lasting, albeit consequent heftiness can make a gynecomastia-like impact. A portion of the advantages of medical procedure incorporate a firmer, compliment, more moulded chest which may give the male patient a lift in fearlessness. There is little downtime, and you may come back to work inside one week normally, unless you are engaged with strenuous exercises.
There will be scar around the areola of the breast (areola) from this system yet will blur over some stretch of time and be less noticeable. There will be some post-agent wounding, swelling, and consuming sensation. To help with the mending procedure, the patient will wear a versatile weight article of clothing for 3 a month and a half and must abstain from presenting scarred zones to the sun for no less than a half year.
Different contemplations incorporate transitory deadness or absence of impression that could last up to a year. Occasional complexities may incorporate contamination, skin harm, liquid collection, dying, and scarring or pigment changes. Post-agent asymmetry, while uncommon, is conceivable; a moment strategy might be expected to expel extra tissue.
Tags: gynecomastia surgery in Jaipur, gynecomastia surgery cost in Jaipur, gynecomastia treatment in Jaipur, Gynecomastia Symptoms in Jaipur, Gynecomastia Causes in Jaipur, Gynecomastia Before And After Surgery in Jaipur, Gynecomastia Surgery Near Me in Jaipur, Treating Gynecomastia Without Surgery, Gynecomastia Removal in Jaipur, How Much Gynecomastia Surgery in Jaipur, Gynecomastia Grades in Jaipur, Gynecomastia Cure in Jaipur, Gynecomastia Doctors in Jaipur, Gynecomastia Post Surgery in Jaipur, Gynecomastia Liposuction in Jaipur, Gynecomastia Reduction in Jaipur, Gynecomastia In Children in Jaipur, Gynecomastia Free Consultation
What is surgery for gynecomastia?
Male gynecomastia is an excessively large breast on one side (unilateral) or both (bilateral). We distinguish :
- The real gynecomastia linked to abnormal development of the mammary gland. The abnormal development of the mammary gland in humans is identifiable by a firm consistency on palpation. More dense, it develops around the areola. Corrective surgery then consists of removing the mammary gland.
- False gynecomastia that contains only fat (adipomastia), more common in overweight men. In this case, corrective surgery involves sucking out the excess fat.
- Because we often see gynecomastia associated with adipomastia, we speak of adipo-gynecomastia. Corrective surgery then consists of liposuction of the excess fat cells and removal of the mammary gland.
A check-up will make it possible to precisely seek the cause of this problem (hormonal imbalance, taking medication). If this is identified, appropriate treatment will be initiated. But sometimes, the origin remains mysterious, we speak of idiopathic gynecomastia
Reconstructive surgery can be performed for the correction of gynecomastia in the event that the cause remains unidentified or the medical treatment has not allowed a total regression of the volume of the breast.
Consultation for correction of gynecomastia
Often benign and frequent, the increase in breast size is however badly experienced, because it damages the image of the male body. Physical discomfort thus goes hand in hand with significant psychological discomfort, sometimes a withdrawal into oneself, particularly in adolescence: the inability to get bare-chested, to go to the beach, to the swimming pool, in the sports locker rooms, to wear clothing close to the body ... Finally, gynecomastia can sometimes be painful.
Its correction is based on medical treatment if the cause is identified, on surgical treatment if the cause has not been found (idiopathic gynecomastia). The Plastic Surgery provides definitive correction of breast hypertrophy and regain a smooth torso.
During the first consultation of at least 30 minutes, the surgeon will carry out an interrogation and a clinical examination allowing to know when the phenomenon appeared, if it is unilateral or bilateral, if the chest is dense or soft (glandular or fatty), if it is accompanied by ptosis (fall with excess skin), if drugs may have induced this gynecomastia (neuroleptics, digitalis, chemotherapy, anti-dopaminergics, estrogen, etc.). Palpation of the testes will eliminate the presence of a nodule… Its examination must ensure that the gynecomastia is not linked to a hormonal pathology ( thyroid disorder , pituitary or adrenal adenoma , testicular cancer …).
A hormonal assessment ( dosage of prolactin , HCG , FSH , oestradiol , LH , testosterone , TeBG, etc.), a renal and hepatic assessment will be necessary. Additional examinations may be requested: x-ray of the lungs , ultrasound of the breasts , testicles, brain MRI ...
After a complete endocrine assessment, with guaranteed income, the surgeon can then explain the most appropriate correction technique and give all the information needed to fully understand the procedure. Now is the time to ask all your questions. The intervention will be prepared using photographs.
The procedure for gynecomastia
BEFORE THE OPERATION
One to two visits with the plastic surgeon are necessary so the plastic surgeon can best answer all of the patient's questions after a thorough examination. The surgeon may request a consultation with an endocrinologist so that a complete assessment can be carried out in search of a cause.
Surgery will only be considered after treatment of the cause has failed or the cause cannot be identified. The surgeon must send a detailed estimate for the operation.
If it is not a remedial intervention, a period of 15 days between the first consultation and the operation must be respected (this is a mandatory reflection period for all acts with aesthetic). Before the operation, a visit to the anesthesiologist at the latest 48 hours before the operation is mandatory.
COURSE OF THE OPERATION
As we have seen, depending on the type of gynecomastia, the operation will first have to either perform liposuction of excess fat, or remove the mammary gland, or both. Secondly, the excess skin will be reduced if necessary. A bandage is placed on the chest after the operation to limit the appearance of edema.
The operation lasts from 20 minutes to two hours depending on the gynecomastia.
The surgery is most often performed on an outpatient basis: over a day without hospitalization.
The operative consequences of a gynecomastia cure
OPERATIVE CONSEQUENCES OF GYNECOMASTIA SURGERY
If it is a simple liposuction, the postoperative pain is minimal, comparable to stiffness. If the mammary gland has been removed, analgesics are needed for the first 24 hours. Bruising and edema will be visible on the operated area. They will slowly subside.
The compression bandage applied at the end of the operation can be removed the next day. It will be replaced by a lighter bandage, or even a compression vest to be worn continuously for several days (to promote skin retraction and healing). Daily disinfection is necessary.
A ten-day work stoppage is recommended. The resumption of sport should not be done before 3 to 4 weeks. Exposure to the sun of the operated area should be avoided in the months following the operation (scar protection can however be provided by a total screen index 50 in the event of exposure). Showering is possible with a mild soap the day after the operation.
Scars depend on the technique used and the quality of the patient's skin. The final result is appreciable after several weeks, after the resorption of the edema, the retraction of the excess skin on the contours of the pectoral muscle.
COMPLICATIONS AND RISKS ASSOCIATED WITH A CURE FOR GYNECOMASTIA
The cure for gynecomastia is now well controlled and complications related to the anesthetic risk and the surgical procedure are rare. Recourse to a surgeon authorized for this type of intervention, registered with the medical council and practicing in a truly surgical context, makes it possible to limit complications and, if necessary, to ensure effective and personalized follow-up. Rare risks are: hematomas (if they are too large, they may require evacuation), phlebitis (very rare in young men), infection (very rare, it may justify reopening and antibiotic treatment), skin damage (exceptional, skin necrosis can leave visible marks. They are favored by smoking),serous effusion (which may rarely require micropuncture), skin sensitivity disorders (most often resolved within a few weeks).
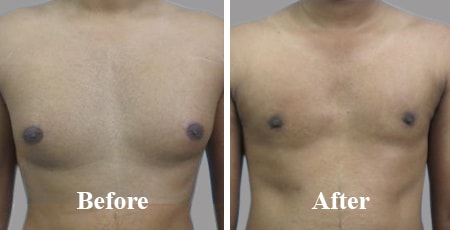
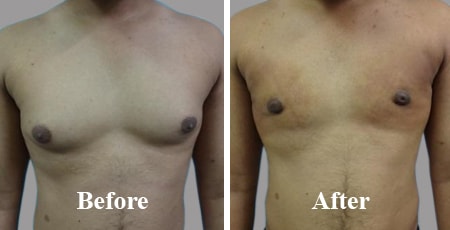
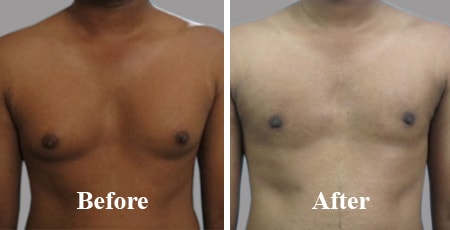
Benefits of gynecomastia surgery (and before / after photo)
The results of a gynecomastia cure are radical and definitive, whether it is glandular gynecomastia (removal of the gland resolves the problem) or fatty gynecomastia (adipocytes not having the ability to multiply). Be careful, however, this operation does not make it possible to save a healthy lifestyle with monitoring of weight gain so that the result of the operation lasts.
The aesthetic benefit is obvious and the psychological benefit also: the patient finds a "male breast".
Result of gynecomastia correction by liposuction and glandular removal. The excess skin was managed by an upper areolar plasty (removal of a skin crescent above the areola for an ascent thereof)
IMPERFECT RESULTS
The benefits are visible quickly. In rare cases, imperfections may be visible: hollows or nodules under the skin following liposuction of excess fat. Massages and hydration of the skin will reduce this phenomenon; temporary insensitivity of the nipples; poor healing with the appearance of a keloid scar may require specific treatment; a concavity of the areola (hollow areola) or a skin surplus: surgical correction may in rare cases be necessary to correct it.
Contraindications of gynecomastia surgery
There are some important contraindications to this surgery:
- If the cause of gynecomastia is identified and can be managed with medical treatment, surgery is not indicated;
- A history of phlebitis or pulmonary embolism may constitute contraindications to this operation;
- Smoking increases the risk of skin necrosis, which can delay healing and delay healing. It is therefore recommended to stop smoking one to two months before the operation and as many after.
Cost of gynecomastia
Social Security coverage of true gynecomastia (therefore glandular or mixed gynecomastia) is possible under certain conditions: when it is an “accused” gynecomastia after puberty, diagnosed after having carried out an endocrine assessment , when it causes psychological or sexual discomfort (more easily recognized in the case of unilateral gynecomastia, pain, etc.).
The price for such an operation can vary from 2500 to 5000 euros. If it is supported, the fees remaining at your expense can nevertheless be reimbursed by the mutual. Check with your surgeon and ask for a prior estimate.
The expert's opinion
Overall, the surgical treatment of gynecomastia and adipomastia is joined, it is just the proportions of excess fat and glandular to be removed that change ...
Indeed, even when it comes to adipomastia, there will always be a glandular component to be treated. In this case, the only correction of the fatty component would risk leaving a glandular residue (hard core behind the areola) which can leave a nipple still prominent, and thus annoying during the summer dressing.
In the context of gynecomastia, removing the gland alone without associated liposuction could lead to an unsightly result with a hollow areola ...
Each time, the treatment should be based on the same principle: the complete correction of any excess fat and glandular, this so that the result is optimal and final.
Finally, the component of excess skin that exists in some cases will need to be managed. The surgeon will take care to avoid any scar that is not hidden around the areola, trusting the retraction capabilities of the skin. In this case, wearing a compression garment (bolero-type compression vest) will play an important role in giving the best chances of skin retraction.
What is gynecomastia?
Definition
Gynecomastia is an exaggerated development of the mammary glands in men. It is a benign but troublesome pathology that is defined as hypertrophy (abnormal increase) of the breast in men. . This increase in the volume of the mammary gland corresponds to unilateral or bilateral hyperplasia (a single breast or both may be affected), gynecomastia may or may not appear symmetrically.
Who is concerned ?
Gynecomastia is a condition that affects men, whether they are teenagers or adults of any age .
There are normal forms of gynecomastia (so-called "physiological" gynecomastia) which affect newborns and young adolescents during puberty. It manifests itself, in this case, in a transient manner ( pubertal gynecomastia ) due to a temporary hormonal imbalance but fades naturally (between 6 months to 2 years in infants and between 16 and 17 years in adolescents).
Also, gynecomastia becomes more frequent with age, from 65 years old, because of the drop in androgenic hormones, it is then considered normal (physiological).
Photo of physiological gynecomastia in adolescents. The hypertrophy of the breast (here mainly glandular) should improve spontaneously between 16 and 17 years
What are the symptoms to be aware of?
The glandular development is characterized by a firm consistency on palpation , we feel a tissue mass distributed concentrically behind the nipple , some patients evoke an impression of swollen nipple, the visual appearance of which is called " areolar protrusion or turgor ". In normal humans, the mammary gland exists but is defined by a simple mammary bud, most of the time impalpable and invisible. In men with gynecomastia, the mammary gland is dense and its development, often painful, is concentrated around the areola. Gynecomastia surgery consists of excising (removing) the mammary gland (most often associated with the removal of fatty masses so that the breast harmoniously matches the pectoral muscles).
Result at 3 weeks of a gynecomastia operation in a man. The correction of the hypertrophy was done by removing the mammary gland using a scar hidden in the areola. The excess fat is systematically removed at the same time by liposuction.
What is the difference between adipomastia and gynecomastia?
We must differentiate between real gynecomastia and adipomastia , also called pseudo or false gynecomastia. More frequent, adipomastia is characterized by a fatty accumulation not centered on the areola and installed on the whole of the breast and therefore increases its volume. The consistency on palpation is soft, diffuse all over the breast and unresponsive . The surgery consists of removing the excess fatty components by liposuction or liposuction (it is systematically associated with the removal of any glandular residue for a lasting result).
Often, gynecomastia associated with adipomastia is observed. We are talking about adipogynecomastia. Surgical treatment is liposuction of excess fat cells combined with removal of the mammary gland.
Result one month after surgical treatment of an aesthetic breast adipomastia. The areola was here ascended by a scar concealed around its periphery. Even if it is an adipomastia, the removal of any glandular residue is systematic for a very flat chest.
Another result at 3 months of an operation for adipo-gynecomastia. The 2 glandular and fatty components have been treated for a harmonious and definitive result
“Having chest” for a man, is it a common problem?
Gynecomastia is a common pathology that is difficult to assume. Indeed, having "breasts" in a man whose male breast is supposed to marry the pectoral muscle, quite often induces a psychological discomfort of great intensity because it constitutes a form of attack on virility that can lead, from adolescence, to withdraw into oneself: the impossibility of getting shirtless in public (at the beach, at the swimming pool, in the sports locker rooms ...), of wearing close-fitting clothes ... In addition to the psychological problems it causes, gynecomastia can be painful sometimes.
Gynecomastia is much more common than one might think since it affects more than half of men and causes discomfort that should not be underestimated. This pathology can be completely corrected, whether it is idiopathic (ie without a cause found) or following an abnormal production of hormones linked to drug treatment or not.
Treatment
Can gynecomastia be treated with medication?
In the presence of a hormonal problem, a simple specific medical treatment before any surgical treatment prescribed by an endocrinologist can help to reduce it, knowing that in case of proven hypertrophy, the effect will be moderate (and only on the glandular excess ..). In cases where no cause is found and the hypertrophy consequent, it is plastic surgery which makes it possible to definitively correct a gynecomastia and to find a harmonious torso.
Other result after bilateral mixed gynecomastia operation
Can cosmetic surgery solve the problem of gynecomastia?
Yes, the results of surgical excision of the gland are radical and definitive in cases of glandular gynecomastia. Indeed, the gland completely removed, will not come back. The same is true for forms with a predominantly fatty component treated by liposuction (the fatty cells called “adipocytes” which do not divide in adulthood). Thus, in the event of an enlarged breast, the complete removal of the gland and the fat will protect the patient for the long term from any recurrence . In addition to physical comfort, the operation of gynecomastia brings to the patient a considerable psychological benefit, the patient finding a male chest, which marries the pectoral muscles.
Surgical correction of moderate bilateral gynecomastia called "areolar turgor". The removal of the gland was accompanied by liposuction for a harmonious and definitive result. The scar, pink at first, is hidden in the areola. It will fade in a few months.
A cosmetic surgery intervention, like any other surgical intervention, always involves a part of uncertainties . The use of a competent and qualified cosmetic surgeon with the National Order of Physicians helps to limit the risks or complications. The plastic surgeon accompanies you before, during and after the intervention by ensuring a conscientious and rigorous postoperative follow-up.
Can bodybuilding overcome gynecomastia?
Weight training cannot solve a problem with gynecomastia because it is a glandular pathology. This physical activity develops the pectoral muscle but unfortunately does not eliminate the mammary gland (which is not subject to hygienic-dietetic measures), nor completely the localized fat (called “lipomerism”) if it is a problem. adipomastia or mixed gynecomastia . Depending on the case, drug treatment (especially in the event of hormonal disruption) or the cosmetic operation can alone overcome it.
Price of gynecomastia
How much does the intervention cost?
The surgeon must send a detailed estimate listing all the points of the intervention (more information on the prices of a correction of gynecomastia ).
In the case of "true gynecomastia", that is to say when there is a true glandular hypertrophy documented by the endocrine assessment, the operation will be covered by the Health Insurance, the coding of the nomenclature of the social security must be indicated (code QEFA 002), the patient will be able to know his level of reimbursement with his mutual. The surgical technique and the methods of hospitalization are explained to the patient.
Is reimbursement possible for gynecomastia?
A support by Social Security exists for a proven gynecomastia ie when the hypertrophy of the breast is consequent and resulting from an excess predominantly glandular (and not fatty). This "real gynecomastia" must be confirmed by the endocrinologist (and the breast ultrasound that he will have prescribed). If these elements are confirmed, the treatment does not require the drafting of a request for prior agreement (and, therefore, the agreement of the medical adviser). The fees of the surgeon and the anesthetist, which remain the responsibility of the patient, can be partially or totally reimbursed by the mutual insurance company depending on the insurance contract taken out. Be careful, however,minimal gynecomastia (certain minor areolar turgorisms) may not present sufficient clinical signs to justify this treatment.
Correction in a man of mixed bilateral gynecomastia (adipogynecomastia) covered by social security. The operation made it possible to treat the areolar turgor (arolar protrusion) and to definitively reduce the volume of the breast (total glandular and fatty removal). The scar becomes almost invisible within a few months.
The operation for gynecomastia
How to prepare for the operation?
We recommend 1 to 2 preoperative visits with the plastic surgeon. It is necessary to first research the origins and possible causes of gynecomastia , the surgical procedure being carried out only after failure of the treatment of the cause (if a cause has been detected). A complete endocrine assessment is prescribed by an endocrinologist in order to rule out any hormonal cause. The intervention strategy is adapted to each patient. A visit with the anesthetist is mandatory more than 24 hours before the operation to prepare for the operation.
How is the operation going?
The duration of the operation for a correction of gynecomastia varies from 20 minutes (adipomastia or fatty gynecomastia ) and sometimes up to an hour for true gynecomastia where the removal of the mammary gland (and systematic fat) must be associated with a correction a significant excess of skin.
Thus, the reduction of the breast in men concerns the fat and the gland, with varying proportions.
The length of hospitalization also varies depending on the case, but it is most often done over a day, on an outpatient basis with an exit in the late afternoon (if the patient does not live too far from the clinic). A bandage (velpeau bands with the wearing of a compressive bolero) is placed all around the chest at the end of the operation to reduce the appearance of edemas.
Distant result of surgical reduction of the breast after treating bilateral mixed gynecomastia in a 35-year-old man
What are the postoperative consequences?
Is it painful?
If it is a simple liposuction, the pains are minimal , akin to simple aches. In the case of an associated gland removal, it is often necessary to take analgesics to soothe the pain during the first 24 hours. Bruises (bruises) and edema appear on the treated area and gradually resolve. Daily disinfection should be performed for the first few days.
How long does the convalescence last?
A work stoppage of a few days is recommended depending on the professional activity. The resumption of sport is done within 3 to 4 weeks depending on the case. For the first few days, for comfort and to limit edema, it will be important not to lift your arms too much and not to carry heavy loads.
On the right, result of an operation aimed at treating the 2 components (fatty and glandular). The convalescence to resume sport is 4 weeks
Are the scars visible?
The scars , inherent in all surgeries, depend on the surgical technique used and the physiological factors of the patient (age, skin quality, skin color, etc.). In almost the majority of cases, they will be hidden around the areola, in the darker pigment.
The final and optimal result of the scar from the gynecomastia operation is appreciable after 10 to 12 months (date of scar maturity). For the form, it will be necessary to wait several weeks, the time for the edema to subside, for the excess skin to retract and for the breast to completely marry the pectoral muscle.
What is gynecomastia?
Gynecomastia corresponds to an excessive development of the male mammary gland, creating an excess of breast that is too raised, or even a sagging female breast. There is frequently an excess of fat associated with it.
Gynecomastia can affect a single breast or both, more or less symmetrically.
The normal breast in men is made up of fat and an almost invisible gland.
In the event of gynecomastia, the breast develops abnormally due to an excessive development of its various components: gland and / or fat.
Typical gynecomastia is a combination of excess gland and fat.
There are many generalist sites that provide quality information on gynecomastia . Through my expertise, I was also able to give my expert opinion on gynecomastia in various articles. Official information on this subject is provided in particular by the French Society of Plastic Surgery in its information sheet on gynecomastia .
Adipomastia
Sometimes gynecomastia consists exclusively of fat overload. This is called adipomastia . The treatment is then very simple and generally relies only on liposuction.
However, by abuse of language, adipomastia and typical gynecomastia are grouped together under the name of gynecomastia , especially since very often, gynecomastia is mixed, that is to say both fatty and glandular.
The right candidates for the treatment of gynecomastia?
You are a good candidate for gynecomastia surgery when you have certain criteria:
- you want to correct the feminine aspect of your breast
- you are uncomfortable being shirtless
- you want to improve your physical proportions
- you suffer psychologically from those feminine or oily breasts that do not go with the rest of your body
- you want to improve your self-confidence
What are the causes of gynecomastia?
Gynecomastia is very common, and most often no cause is found. We are talking about idiopathic gynecomastia.
However, before being able to affirm it, it is necessary to carry out a complete assessment of gynecomastia , to search for a possible pathological or medicinal cause.
It includes an interrogation, a clinical examination, and a blood test. An ultrasound and / or mammogram are often helpful in pinpointing the glandular component of gynecomastia and removing a tumor. I will systematically prescribe this assessment during the consultation.
Among the pathological causes of gynecomastia, that is to say among the diseases that are likely to lead to gynecomastia, we must mention:
- tumors of the testis, adrenal gland, pituitary gland, lung
- Klinefelter syndrome, characterized by the existence in a man of one, two, or three supernumerary chromosomes
- kidney disease, thyroid disease, cirrhosis of the liver
- Testicular hormonal insufficiency
What are the treatments for gynecomastia?
It is always necessary to carry out a preoperative assessment and not to rush especially in adolescents. indeed at puberty gynecomastia is frequent linked to hormonal surges, and it often returns to order spontaneously within 2 years.
Treatment of the cause of gynecomastia
In cases where there is a cause for the gynecomastia, treatment is that of the cause of the gynecomastia. We do not therefore seek to remove the excess breast. Depending on the cause, the treatment will be hormonal or surgical (testicular tumor, etc.). Medications causing gynecomastia will be replaced if possible.
Surgical treatment of gynecomastia
If no cause is found for gynecomastia or if medical treatment has failed in cases where there is a cause, the only way to treat gynecomastia is to remove excess tissue: mammary gland and fat under -cutaneous.
Treatments frequently associated with the treatment of gynecomastia
Gynecomastia often requires associated management of the entire figure. The treatments associated with the treatment of gynecomastia are mainly based on liposuction, but also on all aesthetic procedures for men.
What are the surgical treatments for gynecomastia?
Liposuction
It is the exclusive treatment in cases of adipomastia (exclusively fatty gynecomastia).
Subcutaneous mastectomy for glandular gynecomastia
In glandular gynecomastia, the mammary gland, which is hard, cannot be aspirated by liposuction. It can only be removed surgically. The removal of the mammary gland is called a “mastectomy”.
It all depends on the size of the breast and the elasticity of the skin:
- When the skin is sufficiently elastic, which is the majority of cases, the entire operation can be performed through a short and discreet incision around the areola. Located on the periphery of the lower half of each areola, it represents a small semi-circle.
- On the other hand, when gynecomastia is accompanied by a large excess of skin and it is not elastic, the incisions are horizontal, more or less long, and around the areolas.
A technique that combines 2 steps:
- I systematically perform breast liposuction , and the fatty extension of the breast to the armpit and to the back. Liposuction thins the breast safely in a very simple way. It thus allows to isolate the mammary gland in excess, which will be easily removed by a targeted surgery.
- I then carry out each time necessary, an ablation of the remaining gland by a lower peri-areolar scar .
The advantage of this technique is based on the systematic use of liposuction which:
- reduces surgical detachments
- perfectly delineates the excess gland
- promotes skin retraction
- allows a harmonious and homogeneous treatment of the breast
- shortens the duration of postoperative surgery.
What is the result of gynecomastia surgery?
The result is immediate with a disappearance of the breasts visible from the first dressing the day after the operation.
The final result of gynecomastia surgery is not observed for 6 months to 1 year, in particular due to the progressive nature of skin retraction. On the other hand, from 3 months, the final result is obtained on the fat volume.
The scars around the areola are not visible most often.
Rarely, long chest scars in case of major excess skin are visible, but may be concealed by chest hair.
You have to wait at least 12 months to judge the final appearance of the scars. Several follow-up consultations are carried out, approximately 1 month, 3 months, 6 months and 1 year after the operation.
Price of gynecomastia treatment
The price of gynecomastia depends on two parameters:
- the type of treatment required (liposuction alone, subcutaneous mastectomy, scars around the areola or horizontal scars, etc.)
- possible coverage by social security
What happens before the gynecomastia procedure?
- 2 plastic surgery consultations spaced at least 15 days apart are compulsory before gynecomastia surgery, during which medical photographs are always taken.
- A preoperative mammography is systematic, as well as an endocrine assessment and a testicular ultrasound.
- A bolero-type compressive vest is prescribed.
- Strict smoking cessation 2 months before the operation, to reduce the risk of skin necrosis.
Course of the gynecomastia intervention
The course of the treatment of gynecomastia is based on a well-regulated process, from preoperative consultations to postoperative follow-up.
What is the type of anesthesia for gynecomastia surgery?
Anesthesia is classically a general anesthesia.
The surgical intervention
It takes place in a clinic. The duration of the operation varies depending on the technique used: 1 hour for liposuction, 1 hour 30 minutes for subcutaneous mastectomy, 2 hours for techniques with horizontal scars.
In the event of liposuction, the discharge is the same day (outpatient hospitalization). Otherwise, hospitalization lasts 1 night on average.
Usual post-operative consequences of gynecomastia surgery
- A suction drainage and a compression bandage are put on at the end of the operation. In the event of liposuction, no drainage is placed.
- The length of hospital stay is usually 24 hours.
- Postoperative pain after gynecomastia surgery is usually minimal. In all cases, it is easily controlled by the usual analgesic drugs.
- A compression garment should be worn continuously for one or two months. It aims to apply the peeled skin on his basement.
- The threads are absorbable.
- The prescribed sick leave is usually 5 to 10 days.
- Sport, violent movements, the carrying of heavy loads, are prohibited for one to two months.
What are the risks of gynecomastia surgery?
Fortunately, complications from gynecomastia surgery are very rare.
General complications
These are the risks associated with general anesthesia, thromboembolic accidents (phlebitis, pulmonary embolism), hematomas, exceptional infections.
Complications specific to gynecomastia surgery
- The areola necrosis is exceptional.
- Healing disorder: As with any scar on the body, the course lasts for at least 6 to 12 months, with a phase of redness and initial induration of the scar for 2 to 3 months.
- Unsightly results:
- Insufficient correction of gynecomastia, with residual excess of subcutaneous fat and / or skin
- Concave aspect (hollow) of the breast, related to the thickness of the residual fatty layer around the breast which has been removed. Complementary liposuction can be offered to reduce it
- Too deep appearance of the areola due to excess resection at this level: an injection of fat can correct the problem (lipofilling).
- More or less wrinkled appearance of the chest, when the skin has not retracted sufficiently or correctly. This aspect can only be improved at the cost of a more or less long horizontal scar on the breast, because it is necessary to remove the excess skin
Gynecomastia is a mammary gland that develops in men behind or under the nipples on the chest. However, the problem most often occurs during puberty and continues or worsens into adulthood. In addition, gynecomastia is more common than one might think. The figures show us that more than 40% of men are affected by this problem.
- How can we detect the onset of gynecomastia?
At first glance, gynecomastia can be difficult to spot early in its development. Sometimes a man may develop a reaction of embarrassment or even fear as soon as the first signs of gynecomastia appear. In addition, this discomfort may cause some patients not to expose their bare torso for fear of being ridiculed. In some cases, many will simply refuse to recognize the problem and will look for a way to alleviate the situation by weight training or by favoring loose clothing.
Sometimes, the problem is characterized by the appearance of breasts that can develop to the point of making them appear more feminine. Also, when the gynecomastia is more severe, the patient may even develop tenderness and swelling of the nipples. We will notice an accumulation of pectoral fat (adipomastia), linked to more or less obesity. In addition, adipomastia can develop asymmetrically.
- What are the causes of breast development in men?
Gynecomastia has no specific cause and it can even be multifactorial. For example, it can be caused by obesity, hormonal imbalance, genetic alteration, or taking certain medications. Gynecomastia can develop following the use of anabolic steroids or the consumption of cannabis (marijuana).
- How do I know if I have gynecomastia or adipomastia?
As described above, it may turn out that the development of a breast in men, is a false gynecomastia. In this case, we are talking about a pectoral adipomastia without the presence of mammary gland. In other words, it is more due to the accumulation of fatty tissue in the chest. So the good news is that it can be resolved by combining weight loss with exercise or strength training. We also recommend combining physical activity with a healthy diet and a balanced lifestyle. If these adjustments to your lifestyle do not provide the desired result, liposuction will suffice to extract the excess fatty tissue from the breast.
On the other hand, in the case of gynecomastia there is a development of the mammary gland. This is why it cannot be eliminated by means of weight training or exercise. So, if you think you have gynecomastia, you can do a self-assessment before seeing your doctor. First, you need to raise the arm by placing your hand behind the head. Next, you should feel around the nipple to see if you have a lump behind or under the nipple. If you notice tissue swelling or a hard lump, this is a sign that you probably have gynecomastia.
- What should I do if I have signs of gynecomastia?
In this case, we recommend that you make an appointment for a consultation in order to have a more in-depth examination. Once the diagnosis is confirmed, we will explain the surgery to you.
Note that it is also preferable not to operate in adolescence, because sometimes the gland can resolve spontaneously. On the other hand, in adulthood, it tends to remain stable or to develop quietly.
- At Clinimedspa how do you treat gynecomastia?
Dr Arbor proceeds by means of a lipo-gynecoplasty, which consists first of making a generous tumescence in the tissues (local anesthesia). Then we proceed to liposuction or sometimes only the mobilization of the gland by the lateral incisions (1). The gland is excised in several fragments by the incisions under the nipples (2). This technique developed by Dr Arbor makes it possible to obtain a result that is more aesthetic and as regular as possible. On the other hand, he will sometimes use drains, which are small pears attached to a long tube placed on the side (1). You will need to keep them for a period of a few days to a week in order to collect the liquid. Sometimes, adding skin tightening with radiofrequency is indicated to optimize the result.
- What type of anesthesia is used for lipogynecoplasty?
We perform lipogynecoplasty on an outpatient basis and under local anesthesia with sedation for the comfort of the patient. Once the operation is completed, the patient can return home with his companion just a few minutes after his operation.
- How long does the intervention last?
The surgery lasts an average of 1 to 2 hours depending on the severity of the cases and longer if the procedure is combined with another treatment.
- Is liposuction always necessary?
No, it is not always necessary to have liposuction. This is the case when the patient is very thin and the mammary gland is well localized. In this situation, Dr. Arbor will suggest simply proceeding with mini-incisions (2) under the nipples in order to remove the mammary gland.
- Can we combine the treatment of gynecomastia with other interventions?
Yes, if you wish, we can take this opportunity to combine several interventions. In this case, we can consider combining liposuction or Bodytite treatment in other areas of your body. The most common areas are the abdomen and flanks.
- What is the duration of the convalescence following the intervention?
For most men, the recovery time ranges from a few days to 2 weeks. However, in the case of a very physical job, the convalescence could last up to 4 weeks. After this period, you can go about all of your occupations. During the first 6 months after the procedure, we recommend that you avoid exposing your scars to the sun without protection to avoid the problem of hyperpigmentation of the scars.
- What are the risks of recurrence?
In 2 to 5% of cases, there may be a recurrence of the gland behind the nipple. It would be apparent within 6 months after the operation. Then, Dr. Arbor will have to intervene again under local anesthesia to correct the problem.
Gynecomastia is an abnormal increase in the size of the breast in men, caused by excessive development of the mammary gland or surrounding fat. It can affect a breast, it is then said to be unilateral or both, and is qualified as bilateral. Gynecomastia is defined as enlarged breasts in men.
Before gynecomastia
In order to match the treatment and the interventions to be planned, it is essential to clearly identify the problem. The first step is to perform a mammogram. It will highlight the presence of a tumor nucleus or not. It also defines the composition of the breast, and specifies whether there is an excessive volume of the mammary gland or if it is only a fatty mass.
If the x-ray of the breast reveals a hypertrophic gland , the analyzes are continued with an ultrasound of the testicle: the presence of an abnormal nodule would explain an excessive hormonal production. This examination is combined with a biological assessment to check, among other things, the level of creatinemia, the dosage of prolactinemia, testosterone, LH (luteinizing hormone which stimulates the production of progesterone) and FSH (or stimulating follicle stimulating hormone. estrogen synthesis). A liver workup and palpation of the testes can also identify the problem.
This assessment is prescribed by the attending physician or an endocrinologist. A plastic surgeon can also order this complete endocrine exam. After the workup provides all the necessary information, the surgeon will know what type of operation is needed to bring the problem to an end.
It is essential to consult a specialist before any appearance of gynecomastia for a medical assessment because 1% of breast cancers concern men.
During gynecomastia
If it is mainly fatty gynecomastia , liposuction is the appropriate intervention. In this case, it suffices to make a small incision at the level of the chest. Fat is sucked through this 3mm incision. In the very rare cases where, after aspiration, there is still a significant excess of skin, liposuction can be combined with a breast lift.
If it is glandular gynecomastia , the plastic surgeon begins by speaking with the patient during one or two preparatory visits. This is an opportunity to discuss the course of the operation, the risks to be taken into account and the habits to adopt after the operation. An appointment with the anesthetist is also to be scheduled, in the two days preceding the operation.
The duration of the operation, for an ablation of the mammary gland, is one hour on average (against 30 minutes for a liposuction in case of adipomastia). To achieve this ablation, a resection is performed at the lower hemi-circumference of the areola. The removed mammary gland is sent to an anatomopathology laboratory for analysis.
After gynecomastia
The operation is followed by an outpatient hospitalization during which the patient will keep a bandage around the chest in order to reduce the appearance of edema. One of the main postoperative risks is the appearance of a hematoma.
Within 24 hours of the operation, the patient may experience more or less intense pain, which is calmed with analgesics. Professional activity will only be resumed after ten days, and sport after three or four weeks.
To fully appreciate the results of the operation, it is sometimes necessary to wait two months, the time for healing to be well advanced, or even complete, and for the edemas to subside. At the end of this period, the breast should have perfectly matched the pectoral muscle.
All other non-surgical treatments like creams that can be found on the internet for example have no proven effectiveness.
What is the price of gynecomastia?
For liposuction (to treat mainly fatty gynecomastia), the budget to be expected is 3,000 to 3,500 euros including tax on average.
The prices for an intervention to correct gynecomastia by removal of the mammary gland vary according to a possible coverage by social security. Social Security mentions specific criteria for reimbursement. Three conditions must be met:
- the operation is performed after a complete endocrine assessment
- it takes place on a subject who has passed the puberty phase
- it is a marked gynecomastia which can lead to psychological or sexual problems
The assessment of these criteria is left to the surgeon. The management is codified QEFA 011 for unilateral gynecomastia, and QEFA002 for bilateral gynecomastia. The prices also depend on the extent of the hypertrophy and the specificity of the case. If Social Security agrees to pay for the intervention, it will only be for hospitalization. The fees of the surgeon and the anesthetist remain the responsibility of the patient, because it is a reconstructive surgery.
Photo before and after a gynecomastia procedure
This is a classic case of adipomastia, ie an essentially fatty excess of the chest causing gynecomastia. This type of case can then be treated surgically by a simple liposuction.A single incision of 3mm on each side of the breast allowed to remove 150 grams of pure fat and also allow retraction of the skin at the origin of an excellent result since this patient got rid of his complex permanently.
The answers to your questions about gynecomastia
What are the main forms of gynecomastia?
Gynecomastia can be unilateral or bilateral , depending on whether it affects one or both breasts. It can also be symmetrical or not. Gynecomastia in men is to be distinguished from adipomastia.
In the first case, the consistency of the breast is firm on palpation. The mammary gland presents a higher concentration at the level of the halo. As adipomastia is a fatty mass, the affected breast is much softer.
What are the main causes of gynecomastia?
This abnormal increase can have various origins. In cosmetic surgery, we mainly see patients embarrassed and complexed by their too large breasts. They most often complain of not being able to put on a T-shirt in summer or of going bare-chested in the swimming pool. These are mainly patients with fatty gynecomastia or adipomastia. Excess weight is most often the cause.
The other causes of gynecomastia are most often medical and concern the mammary gland by imbalance between male hormones (testosterone) and female hormones (estrogen):
- Certain cancers such as testicular cancer especially, but also the kidney or the lung which secrete female hormones
- Pathologies of the endocrine glands such as hyperthyroidism or prolactin adenoma are the most frequent.
- Certain drugs such as anabolic steroids found in bodybuilders, but also estrogen (used by transgender people, for example, to paradoxically have breasts)
- Liver disease such as hepatitis, cirrhosis or hepatocellular failure.
- Alcoholism
Man's surgery
Gynecomastia
Definition
Gynecomastia is defined by the increase in the size of the mammary gland in men.
Usually it is idiopathic, that is to say that no cause is found.
However, a complete endocrinological assessment in search of a cause is systematic (see below).
Indications
The increase in breast volume in men, especially during adolescence, can be badly experienced and cause many psychological problems.
This results in difficulties in exposing his torso and clothing problems.
This gynecomastia can also be painful.
There is no age from which to consider a cure for gynecomastia. This depends on the physical but also psychological impact of gynecomastia.
It is still necessary to wait until the end of puberty to consider this intervention
Intervention:
Depending on the extent of gynecomastia and excess skin, 3 types of interventions can be associated:
- Liposuction:
Infra-centimetric incisions hidden in the infra-mammary fold are made.
Aspiration is carried out using a specific cannula connected to a lipoaspirator allowing deep and homogeneous aspiration. The amount sucked obviously depends on the initial excess.
- Glandular resection:
In case of breast bud resistant to liposuction, a lower peri-areolar approach (hidden at the junction between the skin of the breast and the areola) is performed. It allows the resection of the excess gland.
- Skin resection:
In case of large gynecomastia with excess skin, additional scarring may be necessary. It may be a complete periareolar scar or an infra-mammary scar.
Other information about the intervention
- Hospitalization: Conventional 24 hours on average,
- Anesthesia: General,
- Operating time: 1 hour 30 minutes on average (depending on the excess),
- Preoperative examination: 2 legally obligatory consultations with the surgeon, 1 consultation with anesthesia. A complete endocrinological assessment (mammogram, breast and testicular ultrasound, blood hormonal assessment)
- Contraindication: Tobacco considerably increases the risk of complications and infection. It is therefore contraindicated for 15 days before and after the intervention
Operative suites
Variable from one patient to another, the pain is generally not very important and is well controlled by simple analgesics.
- Some bruising and edema may be present for 15 days,
- Dressings and cleaning every 48 hours at home by the patient for 7 days: cleaning with Biseptin and dressing with greasy tulle on the scars,
- The threads are removed at 10 days,
- A rest is advised for 7 to 10 days,
- A compressive garment is to be maintained night and day for 2 months (compressive "Romeo"),
- Sport and heavy lifting is prohibited for 2 months,
- The final result is generally obtained at 3 months,
- Specific care on scars (solar eviction and massage) will be carried out to make them as discreet as possible.
Control visits are carried out at 1 week, 1 and 6 months.
Risks and complications
Fortunately, real complications are very rare following a gynecomastia treatment performed properly.
However and despite their rarity, you must be informed of the possible complications:
- Anesthetic risks:
They will be exposed during the preoperative anesthesia consultation. - Risks associated with the intervention:
- Early:
Thromboembolic accidents (phlebitis, pulmonary embolism): Rare but formidable, they are prevented by an early rise and the prescription of compression stockings or even anticoagulant treatment for 8 to 10 days).
Bleeding: rarely serious except associated coagulation disorders.
Hematomas: exceptional.
Infection: rare after this type of surgery and prevented by intraoperative antibiotics.
Serous effusions: may sometimes require one or more evacuating punctures.
- Late:
Imperfections of result: In some cases localized imperfections can be observed without constituting real complications: insufficient correction, residual asymmetries, surface irregularities. They are generally accessible to liposuction retouching from the 6th month.
Alteration of sensitivity: it is frequent the first months then fades for a return to normal.
Healing abnormalities: the healing process involving random phenomena, it sometimes happens that the scars are not as discreet as expected, which can then take on variable aspects: enlarged, hypertrophic or even exceptionally keloid.