Flaunt your Chest not Boobs
Call now & Get Discount: 8329060384
Best Gynecomastia Surgeon in Ahmedabad Get Male Breast Reduction & Gland Removal from Best Surgeon!
Gynecomastia Male Breast Reduction Clinic in Ahmedabad- Get the best treatment for Enlarged Male Breast, Puffy Nipples in India at very affordable cost. Complete guide on Gynecomastia, Causes, Symptoms, Cure and recovery. Find the best Male Breast Reduction Clinic in Ahmedabad.
Call now & Get Discount: 8329060384
Free Consultation, Best Treatment, Lowest Cost, Easy Finance Available, 100% Result
Gynecomastia Surgery Cost in Ahmedabad Know the Cost of Male Breast Reduction Surgery, Deals & Offers in Ahmedabad
Gynecomastia Cost Depends on?
The cost of Gynecomastia Male Breast Reduction Surgery depends on Surgeon’s Qualification, Operative facilities, Technique of liposuction, Gland excision needed or not, Stay Required or not, Anaesthetist Experience, Type of Compression garment & Post care facilities given to patient.
Please fill the form for exact costing of Surgery in your condition.
Gynecomastia surgery and its cost in Ahmedabad
chest reduction surgery cost, , male breast doctor specialist near me, , gynecomastia surgery in gujarat, , gynecomastia surgery cost ahmedabad, , gynecomastia doctors near me, , gynecomastia surgery cost in ahmedabad, , gynecomastia surgery near me, , gynecomastia doctor, , male breast reduction, , male boobs treatment, , man boobs surgery, , chest surgery, , gynecomastia surgery in vadodara, , gynecomastia surgery in ahmedabad, , gynecomastia surgery cost in gujarat, , men breast reduction, , gynecomastia surgeon near me, , man chest fat, , gynecomastia surgery cost, , गाइनेकोमैस्टिया सर्जरी,
A breast reduction surgery for men is called Gynecomastia surgery in Ahmedabad. During puberty, due to an imbalance of oestrogen and testosterone hormones men’s breast tissue gets swollen in Gynecomastia. However, men’s breasts cannot develop as much as womenbut it affects both the men’s breasts. Gynecomastia is developed when less amount of testosterone or high amount oestrogen is secreted due to which hormones present in the body is changed ina boy during his puberty or older men’s body. Sometimes people might feel embarrassed or impaired of their self-confidence and may have pain due to overdeveloped breasts. The best surgeons are provided in our clinic for gynecomastia surgery in Ahmedabad. Depending upon Grade of Male Breast Enlargement and Technology used, the cost of Gynecomastia Surgery in Ahmedabad varies from ₹35000 to ₹70000.
Candidate for Gynecomastia Surgery
- Depending upon projection and Ptosis of breast tissue gynecomastia can range from grade 1 to grade 3 in men.
- After losing a large amount of weight those men who are having sagging breast.
- Corrective Gynecomastia Treatment is also opted by men who are having Puffy Nipples or sometimes Projected nipples.
- Liposuction can be done for Male Chest Sculpting even in the absence of Gynecomastia.
Intended Result of Gynecomastia
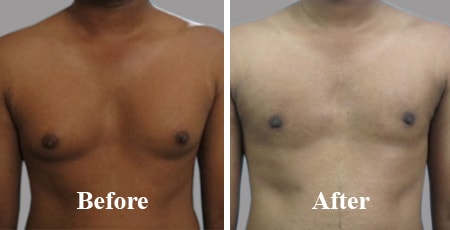
- A flatter chest with a masculine contour with a scar that is almost invisible are the visible results after Correction of Gynecomastia, the breast gland is removed.
Before the procedure
- Your physical health and medical history will be examined by the surgeon before the surgery.
- For getting the satisfying result your desired outcomes have to be discussed with the surgeon.
- The whole procedure about the surgery will be explained by the surgeon after examining your breast.
- To determine the level of hormones, blood or urine samples may be taken by the surgeon for lab testing.
- to determine whether you have a sign of cancer or not, a mammogram of your breast or a sample of tissue will be taken by the surgeon.
The procedure
To make you unconscious, general anaesthesia will be given to you by the surgeon as the surgical procedure starts by giving anaesthesia. To remove excess fatty tissues, liposuction techniques may be used by the surgeon. In this, the cannula will be inserted from small incisions by the surgeon. By move it back to control the motion, the cannula will loosen the excess fat. By vacuum suctionthe excess fat will get removed. To correct the gynecomastia, an excision will be made to remove the excess skin or breast tissue. Areola will be reduced if men’s nipple does not get repositioned naturally, which is necessary. Depending on the condition and preference, the surgeon will use different Incision techniques.
Recovery after gynecomastia
- To be cared for by a friend or relative you are allowed to go home several hours after the Gynecomastia Surgery.
- After Gynecomastia Surgery, usuallyfor 2 to 3 weeks, a compression vest is indicated.
- If needed, to drain off excess fluid, small tubes may be placed near the surgery site but usually drains are not needed in latest male breast reduction surgery.
- After Gynecomastia Surgery, the final results are seen at about 5-6 months for grade 3 Gynecomastia and 2 months for grade 2 Gynecomastia. We see the final results of Grade 1 Gynecomastia very early.
Tags: gynecomastia surgery in Ahmedabad, gynecomastia surgery cost in Ahmedabad, gynecomastia treatment in Ahmedabad, Gynecomastia Symptoms in Ahmedabad, Gynecomastia Causes in Ahmedabad, Gynecomastia Before And After Surgery in Ahmedabad, Gynecomastia Surgery Near Me in Ahmedabad, Treating Gynecomastia Without Surgery, Gynecomastia Removal in Ahmedabad, How Much Gynecomastia Surgery in Ahmedabad, Gynecomastia Grades in Ahmedabad, Gynecomastia Cure in Ahmedabad, Gynecomastia Doctors in Ahmedabad, Gynecomastia Post Surgery in Ahmedabad, Gynecomastia Liposuction in Ahmedabad, Gynecomastia Reduction in Ahmedabad, Gynecomastia In Children in Ahmedabad, Gynecomastia Free Consultation
Gynecomastia is breast enlargement in men or enlargement of the breasts.
Usually, the breasts in men exist but are reduced to an almost impalpable mass behind the areola.
This mass can gradually develop until it reaches a sometimes very large volume (gigantomastia).
Usually symmetrical, gynecomastia is sometimes asymmetrical and must systematically seek breast cancer requiring rapid treatment knowing the difficulty of radiological diagnosis of breast cancer in men.
Gynecomastia can be made up of gland only, fat only (adipomastia) or, more frequently, a mixture of the two.
Depending on age, there are four forms of gynecomastia:
- in adulthood: between 30 and 40 years old, usually no cause found, it is the idiopathic form;
–In adolescence: between 12 and 13 years old;
- in the absence of obesity: it is most often a small turgid mass behind the areola. This form can also be found in athletes doped with anabolics;
- in the presence of obesity: it is then an increase in breast volume due to fat sometimes associated with a small retroareolar nodule;
- it should be noted that this gynecomastia in adolescents will regress spontaneously in 2 or 3 years but is at the origin of a complex and sometimes very important psychological disorders which may require a rapid intervention;
- in infants: occurs frequently (50% of cases) and affects both little girls and little boys. The clinical form is represented either by a small mass remaining localized behind the areola, or extending a little around it. A flow can be associated.
This pathology always regresses quite quickly without treatment;
–At middle age:
–The morphology of gynecomastia is very variable as is its volume. We can find either purely glandular forms, or purely fatty forms or, more frequently, the combination of the two.
–The causes are variable:
–Hormonal deficiency with a decrease in the testosterone level compared to the estrogen level. This is the most common cause;
- you must systematically eliminate the drug causes of gynecomastia:
Finally, it is important to know that alcohol, the usual drugs, and doping products such as androgens, can also be the cause of gynecomastia.
With the exception of the particular form of the infant, in the presence of gynecomastia, clinical, biological and radiological assessments are essential.
The clinical examination:
–Determines the age, personal and family history, the date of onset of gynecomastia and its speed of development, the extent of the physical and psychological discomfort;
- the clinical examination makes it possible to differentiate the small retroareolar turgid gynecomastia from the larger gynecomastias often mixed made up of gland and fat. The experienced surgeon can clearly tell the difference between fat and gland on palpation.
The symmetry will of course be noted because a rapidly evolving unilateral gynecomastia must raise suspicion of breast cancer and perform immediate resection.
The axillary region should also be palpated for lymph nodes.
–The global clinical examination is finally a more targeted examination in search of certain pathologies that may induce gynecomastia.
In all cases, a hormonal assessment will be requested :
- FSH – LH, prolactinemia in search of a pituitary tumor;
- estrogen androgen balance;
- beta HCG;
- hepatic check;
- ACTH and cortisolemia;
- thyroid hormones (T3, T4, TSH);
- urea creatinemia;
The treatment
In infants, no treatment is necessary.
In adolescents:
- in the event of obesity: weight loss can be attempted, which leads to regression of gynecomastia, provided that it is neither too old nor too large. But often, weight loss in adolescents is difficult to achieve and the complex generated by this gynecomastia is often extremely disabling. It is for this reason that I regularly operate on adolescents with this pathology.
In adulthood : it is necessary to eliminate the drug taken, the doping drugs but also always to keep in mind the cancers of the pituitary gland, the breast and the testis.
Treatment by applying a local cream containing is often not very effective.
In the elderly : even if a cause is rarely found, it will always be necessary to eliminate a drug intake and in particular drugs treat certain cancers (prostate, etc.) or HIV, which must then be attempted to modulate.
In general, the treatment is surgical, especially when the gynecomastia is large and bothersome.
The different types of treatment
What are the different types of surgical treatment for gynecomastia:
- in the form of the small retroareolar nucleus: lower hemi-areolar incision and resection of the lesion under assisted local anesthesia and ambulatory;
- in the larger forms, it is necessary to differentiate the pure fatty forms which can benefit from a simple liposuction, and the most frequent forms, that is to say associating fat and gland, which benefit the best from liposuction associated with excision of the gland by lower hemi-areolar incision.
In conclusion, there are two types of surgical treatment:
–Exclusive liposuction;
–Surgical excision of the lesion by skin incision associated with liposuction.
In fact, liposuction is only intended and effective for pure fatty gynecomastia which is, in my experience, very rarely found.
As soon as there is a gland, it cannot be removed by a simple liposuction under penalty of leaving the gland in place, a source of postoperative surface irregularities and especially of recurrence.
Surgical excision is therefore the classic treatment.
The skin incision is located in an arc of a circle with superior concavity on the line circumscribing the areola. This is the inferior hemi-areolar approach.
The gynecomastia lesion is removed by passing in surface in the fat localized just under the skin and in depth, by shaving the deep muscles in particular the Pectoralis major muscle. One-piece ablation of the lesion, in the form of a wafer, is preferable, to the excision of multiple fragments, in order to avoid incomplete resection.
The result must be harmonious, regular and homogeneous, without leaving areas of depression, unsightly skin "waves" and glandular remains, especially under the nipple, a source of recurrence. The contours of the thorax must remain natural and harmonious.
The most suitable technique
I recommend the technique that will be best suited to each of my patients and which can be summarized as follows according to my experience:
- general anesthesia, most often;
- infiltration of at 1% diluted by half under the skin and deep between the gland and the deep muscle;
- superficial and deep liposuction with a fine cannula, even in the case of glandular gynecomastia, in this case tissue detachment than real fatty aspiration;
- lower hemi-areolar skin incision with a scalpel and subcutaneous superficial detachment with scissors of the entire surface of the gland, leaving only a thin layer of subcutaneous fat, of regular thickness;
- deep detachment in front of the muscle, on the deep face of the gland, allowing to remove a kind of tissue plate which will be identified by 2 threads and entrusted to the histologist for anatomo-pathological examination, - liposuction in particular on the peripheral zones of the thorax located outside the glandular cake removed in order to harmonize the shapes and the external contours of the thorax;
- drainage through a suction Redon drain on each side coming out through the armpits and leave in place for a few hours;
- cutaneous suture by joining flaps according to an innovative and personal technique;
- compression bandage, outside the areolar zone, to be worn for 24 hours, date of the first postoperative bandage;
- postoperative compression by bandage is systematic for 10 to 15 days
Small, extremely commonplace gynecomastia often does not require surgical treatment (medical treatment with an androgen-based gel applied topically can be prescribed by the endocrinologist), but the surgical indication arises, after advice from the endocrinologist, when the deformation is significant and / or there is a significant psychological impact.
Surgical treatment varies depending on the type of gynecomastia. The fatty forms (adipomastia) respond well to liposuction (liposuction). The glandular forms require the excision of the glandular nucleus behind the areola through a small incision made on the periphery of the areola, or inframammary. The mixed forms are accessible by liposuction, then by surgical excision of the glandular residue which could not be aspirated by liposuction; a layer of 8 - 12 mm of gland is left, for the vascularization of the areola and the aesthetic appearance. If the skin is in excess and does not retract, or the breast is too ptosis (drooping, with formation of an inframammary fold), a skin lift is necessary, at the cost of a longer scar on the breast .
practical information
Preparation: Antiseptic shower the day before.
Hospitalization time: 24 to 48 hours.
Duration of surgery: 1 hour 30 minutes to 2 hours
Anesthesia: General.
Pain:
Moderate (1 to 3/7) calmed by moderate analgesics in short duration.
Care:
Drain 24 to 48 hours, postoperative compression bandage, then compression garment type bolero for 3 weeks, elbow position to the body for 8 days then gradual lifting of the arms.
Complications: Hematoma, infection, delayed healing, “hollow” by excess excision, necrosis of the areola, altered sensitivity, rare thromboembolic events.
Contraindications: Tobacco, hypertension, poorly balanced diabetes, treatment causing bleeding.
Follow-up: Visit at 8-10 days - check at 2 months, 6 months and 1 year.
Social exclusion: 8 days - Gradual return to sport after 1 month.
Objectives of gynecomastia treatment
This is a procedure for removing excess gland, fat and skin from the male breast. If there is a difference between the two sides, the surgeon always strive for the most symmetrical result possible. Gynecomastia can be partially covered by social security when there is a glandular nucleus objectified by an imaging test.
Preparation for the gynecomastia treatment intervention
Preoperative consultations
A minimum of two consultations is necessary. The surgeon looks for the reasons that push the patient to have the operation and collects all the medical elements essential for the smooth running of the operation. A clinical examination makes it possible to determine with the patient the objectives of the surgery. A hormonal and radiological assessment as well as an endocrinology opinion may be necessary.
Undergo the operation in the best conditions
The patient must be clearly informed of the objectives of the surgery and the scars in order to be operated in the best conditions.
The weight must be stable in the six months preceding the surgical procedure and the body mass index within acceptable limits (less than or equal to 30 kg / m2). If the patient wishes to lose weight, it is necessary to do so before the intervention so as not to compromise the result.
Tobacco is a contraindication to this type of surgery. It is necessary to stop taking nicotine at least four weeks before and four weeks after the intervention (the only authorized substitute is the electronic cigarette without nicotine).
The operation for gynecomastia
Before the block, the surgeon goes into the room to make the markings that will guide him during the operation.
The procedure is performed under general anesthesia. It lasts between one and two hours and varies according to the procedure carried out which can combine liposuction, resection of the gland and in certain cases lifting to treat the excess skin. The surgeon performs the procedure on both sides. The removed gland is sent to the laboratory for analysis.
The sutures used are absorbable and no drainage is put in place except in exceptional cases.
A dry bandage is applied to the scars and a non-reinforced compression bolero in place.
Gynecomastia treatment: postoperative treatment
Hospital stay
If certain conditions are met (proximity to home, possibility of being accompanied, absence of comorbidities), the operation is carried out on an outpatient basis. The patient is summoned on the day of the block a few hours before on an empty stomach and leaves the same day after checking by the surgeon and / or the anesthetist.
In some cases, overnight hospitalization may be necessary. The patient then leaves the day after the operation after the doctor's visit.
Gynecomastia: Postoperative pain?
The intervention is not very painful and paracetamol is sufficient to relieve the discomfort in the vast majority of cases. Analgesics are systematically prescribed.
Gynecomastia cure: scars
The size of the scars depends on the volume of the gland and the presence or absence of skin to be removed:
- In case of moderate excess of fat alone, the scars are very reduced (correspond to the passage of the liposuction cannula)
- In case of moderate excess of gland and fat we add a scar under the areola
- In the event of a significant excess of associated skin, the scars may be more important (at most around the areola and in the breast fold)
Early post-operative instructions
Scars should be washed daily in the shower with soap and water running off before being dried with a clean towel. The dressing can be unwrapped before or during showering.
At the end of the toilet, care is carried out daily at home by the patient himself or by a nurse according to a protocol established by the surgeon. Finally, the support bolero is placed over the dressings. The latter must be washed regularly (there is no consequence in not wearing it for two hours during the day).
The first follow-up appointment takes place after one to two weeks.
Remote postoperative instructions
The compression bolero is worn for a month in total, day and night.
Sun protection for scars is essential in the year following the operation.
After one month postoperatively to reduce the risk of visible scars, massages can be performed (two per day for five minutes and for a period of at least three months) with a moisturizer. The alternative of silicone dressings can be interesting and should be discussed with the surgeon.
Checks are carried out one month, three months and one year postoperatively.
The results of the analyzes carried out during the operation are given to the patient during the follow-up consultations.
The final result of the intervention can be appreciated three to six months later due to the postoperative edema.
Gynecomastia: postoperative precautions
Resumption of physical activity is only possible one month postoperatively in the absence of healing problems.
Sauna, hammam, baths including swimming pools or sea water are only possible after complete healing one month after the procedure.
Additional information on the treatment of gynecomastia
Possible complications
As with any surgical procedure, a complication can occur (hematoma, infection, disunity, unsightly scars or even keloids).
Gynecomastia: prices
In some cases, the intervention may be partially covered by Social Security when there is a glandular nucleus on ultrasound. No prior agreement is necessary and the indication is asked by the surgeon.
For other cases, it is cosmetic surgery not reimbursed. The estimate will depend on several parameters (choice of the care structure, the complexity of the surgery, any associated procedures) and will be provided to the patient in consultation.
An approximate price list is available on the site.
Work stopping
When the intervention is covered by health insurance, a work stoppage may be justified. The duration of this depends on the arduous nature of the job and generally lasts two to four weeks.
Areola and nipple tenderness
Sensitivity disorders after a cure for gynecomastia are frequent. In the vast majority of cases, these disorders will disappear or greatly diminish after surgery.
The recidivist
It is rare but gynecomastia can recur. A new intervention is then necessary.
What is gynecomastia?
Gynecomastia is an excessive development of the breasts in men, on one side or on both sides, symmetrically or not.
It usually has little or no pain, but sometimes it can be accompanied by tenderness in the chest.
Theoretically, true gynecomastia is related only to the mammary gland, and false gynecomastia contains only fat .
In practice, the two components, glandular and fatty, are very often associated.
Gynecomastia is very common, especially at certain periods of life: in newborns (60% of cases), then at the time of puberty (60% of cases) where it generally disappears in less than two years. In adult men, gynecomastia occurs in about 30% of cases (up to 60% of cases after 70 years).
Why have gynecomastia for men?
In the vast majority of cases, gynecomastia is normal , or "physiological" or "idiopathic", ie no cause is found. However, before being able to affirm it, it is necessary to carry out a complete assessment, in search of a possible pathological or medicinal cause. This assessment must be carried out by an endocrinologist. It includes an interrogation, a clinical examination, and a blood test. Ultrasound and / or mammography are often helpful in specifying the glandular component and removing a tumor.
Among the pathological causes, that is to say among the diseases which are likely to lead to gynecomastia, it is necessary to quote:
- tumors of the testis, adrenal gland, pituitary gland, lung
- Klinefelter syndrome, characterized by the existence in a man of one, two, or three supernumerary X chromosomes
- kidney disease, thyroid, cirrhosis of the liver
- Testicular insufficiency (hypogonadism)
Among the drug causes, that is to say among the drugs which are likely to cause gynecomastia, it is necessary to quote: estrogens, cimetidine.
What are the treatments after the operation?
When a cause is found, it is of course that which must be treated as a priority.
The surgical treatment of gynecomastia in Ahmedabad is particularly aimed at forms that are bothersome by their size or sensitivity, as well as psychologically poorly tolerated gynecomastia. In adolescents, it is necessary to wait about 2 years of evolution before considering surgery.
Liposuction is a method that can only be considered on its own if the content of the breasts consists solely of fat (false gynecomastia).
In true gynecomastia, the mammary gland, which is hard, cannot be aspirated. It can only be removed surgically. It all depends on the size of the breast and the elasticity of the skin.
- When the skin is elastic, and the breast is not too big, which is the majority of cases, the entire operation can be performed through a short and discreet incision. Located on the periphery of the lower half of each areola, it represents a small semi-circle.
- On the other hand, when there is a large excess of skin and it is not elastic, the incisions are horizontal, more or less long, located at the areolas.
- Finally, in the case where the volume of the breasts is very large, the horizontal incisions are located low, and the areolas are amputated and grafted.
Detailed intervention
- Surgical treatment for gynecomastia is an intervention covered by social security, without prior agreement, provided that it is "carried out after endocrine assessment, after puberty, for accused gynecomastia, in the event of asymmetric, painful gynecomastia, with areolar distension ”.
- You can enter the aesthetic clinic in Ahmedabadeither the day before the operation before 5 p.m. or the morning of the operation.
- The operation is performed under general anesthesia. It lasts from 1 to 2 hours.
- A suction drainage (redons) as well as a compression bandage are put on at the end of the operation.
- The length of hospital stay is usually 2 to 4 days.
- Drains do not prevent exit if possible
- Postoperative pain is usually minimal. In all cases, it is easily controlled by the usual analgesic drugs.
- A compression garment (bolero) must be worn continuously for one or two months. It aims to apply the peeled skin on his basement.
- The threads are removed between the 10th and the 20th day after the operation.
- The prescribed sick leave is usually 2 to 3 weeks.
- Sport, violent movements, the carrying of heavy loads, are prohibited for one to two months.
- Follow-up consultations are necessary until the stabilization of the result, which can only be appreciated after 6 to 12 months.
What are the consequences of gynecomastia?
Excessive development of the mammary gland in men is often accompanied by complexes. People are reluctant to wear tight-fitting clothing like T-shirts, shirts, and let alone swimwear. The intimate life can be disrupted because a voluminous chest is often associated with the idea of femininity. A gynecomastia treatment in Ahmedabad makes it possible to permanently remedy this type of problem. Man gynecomastia can be caused by multiple factors. This increase in the mammary gland may affect both breasts or only one. This symptom appears frequently in boys during adolescence but goes away in most cases. This is why this intervention is rather reserved for adults, when the body has completed its full development. Male gynecomastia is also a phenomenon linked to aging, which is why this problem is common in older men and is thought to be due to a drop in testosterone levels.
Why resort to an operation for breast enlargement in Ahmedabad?
The gynecomastia treatment in Ahmedabadmay consist of simple liposuction or may require an operation. Before considering a surgical operation in Boulogne, it is important to look for the causes at the origin of this problem, so as to rule out the existence of underlying pathologies. It is possible to benefit from a reimbursement by social security and complementary health insurance in certain cases, in particular when the gynecomastia causes a strong psychological suffering, that it is accompanied by physical pain or that it produces a strong asymmetry. Your surgery will provide you with a non-binding quote. You can send it to your complementary health insurance, who will tell you the amount of possible coverage. Even if the results are not immediately visible,the operation quickly provides a better comfort of life in most cases. The torso regains a more masculine aspect. The psychological benefit is often significant. If the gynecomastia is of fatty origin, it is important to adopt a good hygiene of life because any increase in weight can cause a return of the mammary hypertrophy.
Can we have gynecomastia surgery in Ahmedabad?
A surgical operation in Ahmedabad offers all the guarantees of safety and reliability. A reduction in male gynecomastia should always be performed in a surgical office specializing in cosmetic and plastic surgery. An operation of the mammary glandis always delicate and must be carried out under conditions of maximum hygiene and safety. A gynecomastia treatment in Ahmedabad must always be accompanied by an adapted follow-up, whether it is to establish a precise diagnosis, to propose an adapted solution or to answer all the questions of the patient. If you wish to carry out this surgical operation in Boulogne, Dr Staub's surgery is able to provide you with all the information you need to make an informed decision. You will be informed in all objectivity about what this operation can bring you and you will be able to assess the advantages and disadvantages. Do not hesitate to ask Dr Staub for advice, he will answer your questions frankly.
Gynecomastia is defined by the appearance of a real breast in men. It can be unified or bilateral. An intervention makes it possible to definitively get rid of this real disgrace, which is often very difficult to assume.
The breast is indeed the symbol of femininity. If the mammary gland does exist in normal men, it is reduced to a simple breast bud and does not form any real relief.
Also when a man notices that he has "breasts" where you should see his pecs, it almost becomes a questioning of his virility, especially if this gynecomastia appears during adolescence, an age at which it is particularly bad. lived.
We must distinguish true gynecomastia from adipomastia which is made up of fat. But very often these are mixed forms called adipo-gynecomastia.
Usually there is no cause for this gynecomastia; she is said to be idiopathic. However, in some cases, it is due to a hormonal imbalance, or related to a testicular or pituitary tumor. Finally, certain drugs can be responsible for this gynecomastia. A review will therefore be necessary before any intervention. In the absence of a found cause, the patient can then be offered a surgical treatment, called a cure for gynecomastia.
Principles of gynecomastia treatment
The goal of this surgery is to restore normal anatomy as well as possible with the following principles:
- reduce the breast volume by liposuction for fatty forms or by direct surgical excision (subcutaneous mastectomy) for glandular forms, or in cases of mixed forms, by combining the two techniques.
- reduce excess skin: generally, the decrease in glandular volume will allow skin retraction, especially in young men who have elastic skin. But in some cases, when the skin excess is too important, it is essential to resect the excess skin at the cost of scars. This skin reduction plasty can be performed from the first intervention or secondarily.
Indications for gynecomastia treatment
Who is gynecomastia treatment for?
Surgical treatment is for all men who present with gynecomastia.
The intervention can be practiced even on the adolescent, with the authorization of the parents; it is even strongly recommended, because of the psychological disturbances it can cause.
Consultation
The clinical examination assesses the development of the mammary gland centered on the areola, most often bilateral and symmetrical, of firm consistency and sensitive to palpation. Gynecomastia should be distinguished from adipomastia which is much more frequent and corresponds to a local accumulation of fat. These adipomasties have a softer bilateral, symmetrical consistency, but the two can be associated (adipogynecomastia).
In adolescents, transient gynecomastia can appear, linked to a hormonal imbalance in favor of estrogen, which disappears within a few months.
Breast ultrasound and mammography will be prescribed to determine the composition of this gynecomia: fat, gland or mixed structure and also to remove a breast tumor.
Indeed, it is the nature of this gynecomastia that will depend on the treatment method:
- isolated liposuction in the event of predominantly fatty gynecomastia,
- treatment by reduction of breast volume by direct surgical excision (subcutaneous mastectomy) in the case of glandular gynecomastia,
- finally combination of the 2 methods in case of mixed gynecomastia
All the information you need to understand your treatment will be provided to you during this consultation. Documents will be given to you so that you can read at home the elements essential to your decision and be able to ask additional questions during the next consultation, which will be free.
Post-operative advice and prescriptions are summarized in a personalized sheet.
Partial support by social organizations for the treatment of gynecomastia is possible under certain conditions: "intervention carried out after endocrine assessment, after puberty, for marked gynecomastia, which may pose a problem of a sexual or psychological nature (in particular asymmetric gynecomastia). , painful, with areolar distension) ”.
The additional fees will be submitted to you in a quote; they are refundable, in whole or in part, by your complementary mutual, depending on the contract you have taken out.
A blood test is carried out as well as a radiological assessment of the breasts (ultrasound, mammography). A preoperative anesthetic consultation is scheduled at least 48 hours before your entry; the anesthetist will explain all the modalities of his gesture to you.
Quitting smoking is strongly recommended; any medicine containing aspirin is prohibited. You will arrive at the clinic on an empty stomach for more than 6 hours.
The intervention
The course
Tracks
The tracings of the incisions and the identification of the breast areas are made in the operating room. Photographs are also taken.
Anesthesia
A "vigil" anesthesia (local anesthesia deepened by tranquilizers administered intravenously is possible for an isolated liposuction. Otherwise it is a classic general anesthesia.
The final choice will be the result of a discussion between you, the surgeon and the surgeon. anesthetist.
Gestures
Doctor, cosmetic surgeon in Ahmedabad, adopts a technique which is specific to her and which she adapts to each case to obtain the best results. However, we can retain basic principles common to any treatment of gynecomastia.
In the case of predominantly fatty gynecomastia, the treatment is isolated liposuction. The scars are then minimal.
In the event of predominantly glandular gynecomastia, a mastectomy is required (resection of the mammary gland). An incision is made at the lower edge of the areola to remove the mammary gland (subcutaneous mastectomy). A drain can be put in place.
In the case of mixed gynecomastia, the 2 methods are combined, starting with liposuction.
Finally, if the excess skin is too large with a skin that is not very elastic, it will have to be resected. The residual scars will have a location and a variable size depending on the case (periareolar, horizontal in the inframammary fold or in T). We can also practice an areola reduction.
A suction drainage and a compression bandage are put on at the end of the operation. In case of liposuction, no drainage is placed.
Finally, a "modeling" dressing is made, often with an elastic bandage or a compression vest.
The duration of the operation is highly variable, depending on the technique used, ranging from 30 minutes in the case of isolated liposuction to over two hours for complex forms requiring major skin reduction.
The stay in the clinic depends on the surgical technique used. For liposuction, the operation can be performed on an "outpatient basis", that is to say with an exit the same day after a few hours of monitoring. Otherwise the hospitalization is 24 hours.
Associated interventions
In case of fatty gynecomastia, abdominal liposuction is sometimes performed at the same time.
Operative consequences of the treatment of gynecomastia
In the immediate aftermath, postoperative pain will be relieved by analgesic treatment. Edema (swelling), bruising (bruising), and discomfort with raising the arms are common in week 1.
The bandage is changed regularly and the compression vest worn day and night for 3 to 4 weeks. This retention helps skin retraction and promotes uniform healing.
A work stoppage of a few days is necessary.
The threads are absorbable.
Certain post-operative care such as massages may promote skin retraction.
It is advisable to wait 3 to 4 weeks before resuming any intense physical activity or sport.
The patient's compliance with the instructions given by the surgeon is essential,
Doctor guarantees you a conscientious and considerate personalized follow-up. You can reach her at any time, 24 hours a day, for any post-operative question.
Post-operative consultations are included in the quote.
The results
Surgical progress and current techniques for treating gynecomastia now allow natural and aesthetic results to be obtained, while avoiding postoperative risks as well as complications as much as possible.
The improvement is immediately visible from the first days but a period of two to three months is necessary to assess the final result. This is the time required for good skin retraction and the disappearance of postoperative edema. Beyond this period, the tissues will gradually gain flexibility.
The thorax becomes flat again.
The tenderness of the nipples gradually reappears.
The scars evolve during one year after the intervention It is imperative to protect them from the sun during the first year.
The result is definitive, but in the event of adipomastia, it is necessary to avoid gaining weight.
The reduction in breast volume brings physical comfort, especially when getting dressed. Finally, the result is often very beneficial on the psychological level because gynecomastia is often considered as a shadow to virility.
Doctor performs the procedure herself and provides post-operative follow-up; she will be able to support you throughout your project, before, during and after the operation.
In conclusion, the treatment of gynecomastia is a reliable intervention which in the vast majority of cases gives very good or excellent results in terms of functional, aesthetic and psychological benefits.